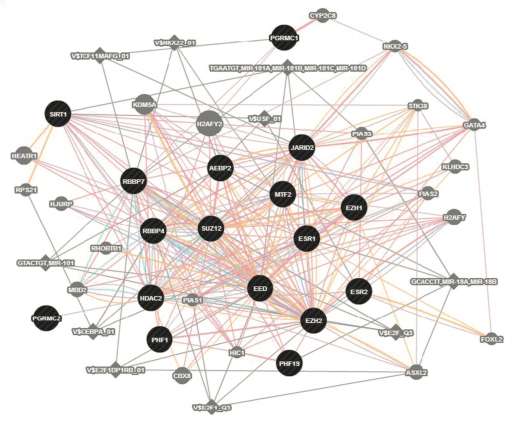
Expression of the ESC/E(Z) gene network was found to be systematically disturbed in PMDD. Credit: Peter Schmidt, M.D., NIMH., David Goldman, M.D., NIAAA
National Institutes of Health (NIH) researchers have discovered molecular mechanisms that may underlie a woman's susceptibility to disabling irritability, sadness, and anxiety in the days leading up to her menstrual period. Such premenstrual dysphoric disorder (PMDD) affects 2 to 5 percent of women of reproductive age, whereas less severe premenstrual syndrome (PMS) is much more common.
"We found dysregulated expression in a suspect gene complex which adds to evidence that PMDD is a disorder of cellular response to estrogen and progesterone," explained Peter Schmidt, M.D. of the NIH's National Institute of Mental Health, Behavioral Endocrinology Branch. "Learning more about the role of this gene complex holds hope for improved treatment of such prevalent reproductive endocrine-related mood disorders."
Schmidt, David Goldman, M.D., of the NIH's National Institute on Alcohol Abuse and Alcoholism, and colleagues, report on their findings January 3, 2017 in the journal Molecular Psychiatry.
"This is a big moment for women's health, because it establishes that women with PMDD have an intrinsic difference in their molecular apparatus for response to sex hormones - not just emotional behaviors they should be able to voluntarily control," said Goldman.
By the late 1990s, the NIMH team had demonstrated that women who regularly experience mood disorder symptoms just prior to their periods were abnormally sensitive to normal changes in sex hormones - even though their hormone levels were normal. But the cause remained a mystery.
In women with PMDD, experimentally turning off estrogen and progesterone eliminated PMDD symptoms, while experimentally adding back the hormones triggered the re-emergence of symptoms. This confirmed that they had a biologically-based behavioral sensitivity to the hormones that might be reflected in molecular differences detectable in their cells.
Following up on clues - including the fact that PMS is 56 percent heritable - the NIH researchers studied the genetic control of gene expression in cultured white blood cell lines from women with PMDD and controls. These cells express many of the same genes expressed in brain cells - potentially providing a window into genetically-influenced differences in molecular responses to sex hormones.
An analysis of all gene transcription in the cultured cell lines turned up a large gene complex in which gene expression differed conspicuously in cells from patients compared to controls. Notably, this ESC/E(Z) (Extra Sex Combs/Enhancer of Zeste) gene complex regulates epigenetic mechanisms that govern the transcription of genes into proteins in response to the environment - including sex hormones and stressors.
More than half of the ESC/E(Z) genes were over-expressed in PMDD patients' cells, compared to cells from controls. But paradoxically, protein expression of four key genes was decreased in cells from women with PMDD. In addition, progesterone boosted expression of several of these genes in controls, while estrogen decreased expression in cell lines derived from PMDD patients. This suggested dysregulated cellular response to the hormones in PMDD.
"For the first time, we now have cellular evidence of abnormal signaling in cells derived from women with PMDD, and a plausible biological cause for their abnormal behavioral sensitivity to estrogen and progesterone," explained Schmidt.
Using cutting edge "disease in a dish" technologies, the researchers are now following up the leads discovered in blood cell lines in neurons induced from stem cells derived from the blood of PMDD patients - in hopes of gaining a more direct window into the ESC/E(Z) complex's role in the brain.
More information: Dubey N, Hoffman JF, Schuebel K, Yuan Q, Martinez PE, Nieman LK, Rubinow DR, Schmidt PJ, Goldman D. The ESC/E(Z) complex, an intrinsic cellular molecular pathway differentially responsive to ovarian steroids in Premenstrual Dysphoric Disorder, Molecular Psychiatry, January 3, 2016, DOI: 10.1038/mp.2016.229
Journal information: Molecular Psychiatry
Provided by National Institutes of Health