New treatment causes cancer cells to fill up with cellular 'trash' and self-destruct
The genomes of cancer cells—cells that do not obey signals to stop reproducing—are riddled with genetic mutations, causing them inadvertently to make many dysfunctional proteins. Like all other cells, cancer cells need to be vigilant about cleaning themselves up in order to survive. Now, biologists in the laboratory of Ray Deshaies, Caltech professor of biology and Howard Hughes Medical Institute Investigator, have developed a new way to inhibit the cancer cell cleanup mechanism, causing the cells to fill up with defective proteins and thus self-destruct.
The findings appear online in a paper in the February 27 issue of Nature Chemical Biology.
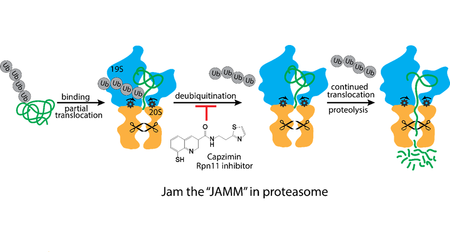
The proteasome is a hollow cylindrical structure that serves as a kind of cellular garbage disposal. It lets in proteins through small openings on each end, chops them up, and spits out the remains. When a bad protein is made by a cell, the protein gets tagged with chains composed of at least four copies of a small protein called ubiquitin. The tags signal to the proteasome that the bad protein needs to be destroyed. One part of the proteasome, called Rpn11, cuts off the ubiquitin chain as the defective protein is being stuffed into the garbage disposal. This step is necessary because the ubiquitin chain is too big to fit inside the proteasome.
A new compound developed by the Deshaies group, in collaboration with researchers from UC San Diego, inhibits Rpn11 activity, making it impossible for the proteasome to fully destroy bad proteins. Massive accumulation of these bad proteins causes catastrophic stress to the cell that results in cell death.
While the compound affects the proteasomes in all cells, normal cells are thought to produce fewer dysfunctional proteins than cancer cells. Some types of cancer cells are therefore more sensitive than normal cells to proteasome inhibition and thus even a small dose of the drug can be fatal to them.
"All current cancer drugs that target the proteasome work by inhibiting the protein-chopping enzymes on the inside of the proteasome; therefore they all have similar drawbacks and tend to lose efficacy over time," says Jing Li, a postdoctoral scholar in biology and biological engineering and first author on the paper. "Our research offers an alternative path to disabling proteasome function, including in cells that no longer respond to the existing drugs."
The compound was tested in human cancer cells in the laboratory, but more work needs to be done to further improve its potency and to evaluate its potential as a therapeutic drug through testing in animals.
More information: Capzimin is a potent and specific inhibitor of proteasome isopeptidase Rpn11. Nature Chemical Biology, nature.com/articles/doi:10.1038/nchembio.2326


















