Migrants at risk of drug-resistant TB in Europe
In the late 19th century, an estimated one in seven Europeans was dying of tuberculosis, then known as "consumption" for its slow, remorseless wasting of the human body.
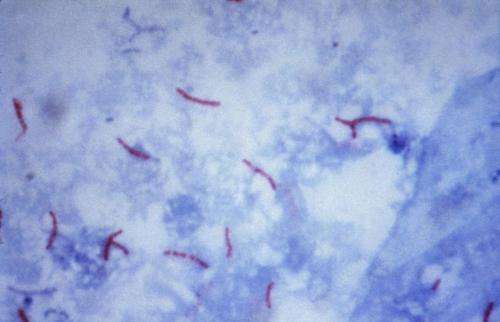
Now, after decades of low TB rates thanks to antibiotics and strong public health systems, the continent is threatened by a new and different form of the lung disease—one which cannot easily be cured with existing drugs.
And the people most at risk, experts say, are migrants and refugees who often find themselves in densely-populated, unsanitary, disease-favourable conditions similar to those blamed for Europe's Victorian era "Great White Plague".
"Although rare in European countries, the risks posed by the current migrant crisis makes MDR-TB (multi- drug-resistant tuberculosis) an important and urgent health priority," the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) said in a recent statement.
And it warned there was a "human rights obligation" to improve the diagnosis, treatment and prevention of drug-resistant tuburculosis in migrants.
Infections on European soil were mainly among migrants themselves, and public health experts stress they should be viewed as a vulnerable group in need of help—not disease spreaders.
A hundred percent of MDR-TB cases in Austria, the Netherlands and Norway were diagnosed in migrants and refugees, said the ESCMID, and around 90 percent in Britain, France, Italy and Germany.
This represented just over 1,400 cases in 12 countries in 2014.
Access denied
Some migrants may arrive already sick with MDR-TB, others with a latent, unobserved infection.
Some may catch these dangerous germs on overcrowded refugee boats or in work or migrant camps.
"Migrants are among the most susceptible groups to tuberculosis," Michel Kazatchkine, the UN secretary-general's special envoy on HIV/AIDS in Eastern Europe and Central Asia, told AFP.
"Most of them acquire a disease in the host country," he said.
Drug-resistant TB strains are more difficult and expensive to treat.
Symptoms are not immediately visible, and the disease can spread easily from one person to another via coughing, sneezing, or simply talking.
But many cases may never be spotted, as European countries do not have a standardised approach to screening.
Migrants may be refused access to treatment or may not know how to, and others might want to avoid a positive diagnosis for fear of being deported.
"The situation in Europe is such that governments are now tightening up in terms of who is able to access free statutory health services," Sally Hargreaves of the International Health Unit at Imperial College London, told AFP.
In 2015 alone, Europe received a million migrants from war-torn countries in Africa and the Middle East.
"There's very little evidence to suggest that migrants pose a major threat to the general population of a country they go to in health terms," Nicholas Beeching of the ESCMID's Study Group on Infections in Travellers and Migrants told AFP.
"Nevertheless, of course it presents a challenge because we want to identify people with MDR-TB and make sure that they get appropriate treatment and also make sure it doesn't spread within their own community... and the general community."
Pre-antibiotic era
In 2015, about half-a-million people worldwide developed MDR-TB and the even more resistant strain XDR-TB, according to the World Health Organization.
One in five were in the WHO's European region, which comprises 53 countries including from hard-hit eastern Europe and Russia.
Treatment was successful in under half of MDR-TB patients and less than a third for XDR-TB—a rate which "approximates that... seen in the pre-antimicrobial era," the journal Clinical Microbiology and Infection warned in its March edition.
"If drug resistance increases substantially, TB elimination will become more difficult if not impossible, to achieve."
TB, an infection of the lungs that can be deadly if untreated, killed some 1.8 million people worldwide in 2015 and infected 10.4 million.
It remains the top infectious killer worldwide—particularly in Asia, Africa and Eastern Europe, which also has the most MDR-TB cases.
MDR-TB does not respond to the two most potent TB drugs—isoniazid and rifampin, and XDR-TB to an even longer list.
"While anyone can contract TB, the disease thrives among people living in poverty, communities and groups that are marginalised and other vulnerable populations," the WHO says in a message for World TB Day on Friday—migrants and refugees among them.
"Addressing the health needs of the disadvantaged, the marginalised, those out of reach of the health system, will mean improving access to health services for everyone."
© 2017 AFP
















