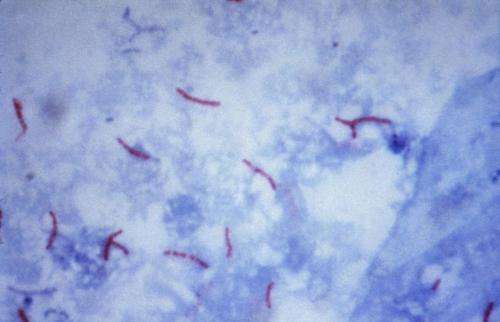
This photomicrograph reveals Mycobacterium tuberculosis bacteria using acid-fast Ziehl-Neelsen stain; Magnified 1000 X. The acid-fast stains depend on the ability of mycobacteria to retain dye when treated with mineral acid or an acid-alcohol solution such as the Ziehl-Neelsen, or the Kinyoun stains that are carbolfuchsin methods specific for M. tuberculosis. Credit: public domain
(Medical Xpress)—A team of researchers from Sweden, France, Belgium and Switzerland has found a way to reverse resistance to an antibiotic drug used to treat tuberculosis. In their paper published in the journal Science, the team describes how they screened compounds that activated different pathways to activate ethionaide, a compound used to treat tuberculosis.
The development of antibiotics to treat bacterial infections has very clearly made the world a healthier place. Unfortunately, over time, bacteria have been evolving to thwart such compounds, putting us all at risk once again. Because of that, scientists have been searching for new treatments, or in some cases, ways to make old treatments work again using new techniques. In this new effort, the researchers have found a way to make ethionaide, a prodrug (a compound that is metabolized in the body to produce a desired drug), become effective again in patients infected with resistant strains of Mycobacterium tuberculosis.
Ethionaide was developed back in the late 1950s as a treatment for tuberculosis. It is activated by an enzyme called EthA found in the bacteria—once activated, ethionaide attacks the bacteria. Over time, many strains of M. tuberculosis have become resistant to ethionaide by developing EthA mutations that do not activate the compound, making it useless as a treatment. To get around this problem, the researchers searched for and found a prototype molecule called SMARt-420 that activates ethionaide by taking a different route—interacting with a secondary gene. The team has found that giving patients a dose of the small molecule after administering a dose of ethionaide restored the lattter's ability to destroy a range of M. tuberculosis—testing showed it reduced the bacterial load found in patient lungs after just three weeks—similar to the effectiveness of ethionaide alone against M. tuberculosis prior to the develop of resistance.
The researchers are currently working with GlaxoSmithKline and Biotech Bioversys to further develop the small prototype molecule into a drug that can be mass produced and sold. They are also looking into the possibility of using the same or a similar technique to overcome resistance to other bacteria.
More information: Nicolas Blondiaux et al. Reversion of antibiotic resistance inby spiroisoxazoline SMARt-420, Science (2017). DOI: 10.1126/science.aag1006
Abstract
Antibiotic resistance is one of the biggest threats to human health globally. Alarmingly, multidrug-resistant and extensively drug-resistant Mycobacterium tuberculosis have now spread worldwide. Some key antituberculosis antibiotics are prodrugs, for which resistance mechanisms are mainly driven by mutations in the bacterial enzymatic pathway required for their bioactivation. We have developed drug-like molecules that activate a cryptic alternative bioactivation pathway of ethionamide in M. tuberculosis, circumventing the classic activation pathway in which resistance mutations have now been observed. The first-of-its-kind molecule, named SMARt-420 (Small Molecule Aborting Resistance), not only fully reverses ethionamide-acquired resistance and clears ethionamide-resistant infection in mice, it also increases the basal sensitivity of bacteria to ethionamide.
Journal information: Science
© 2017 Medical Xpress