Scientists find possible Achilles heel of treatment-resistant cancers
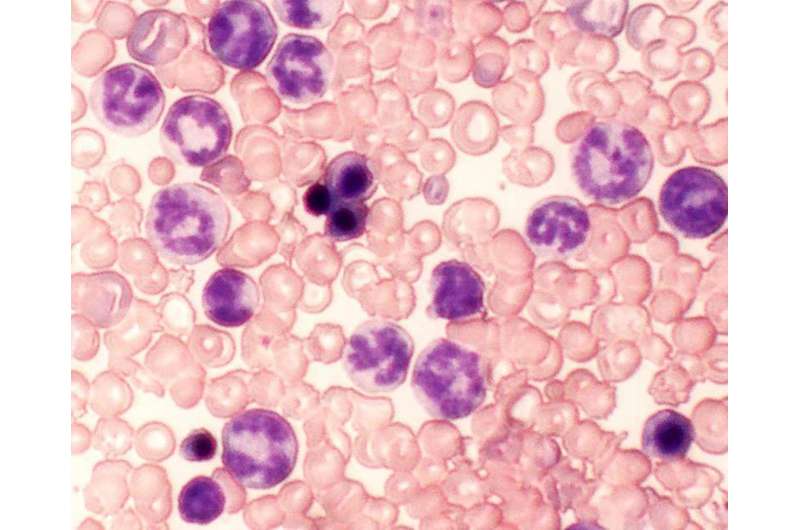
Scientists identify two signaling proteins in cancer cells that make them resistant to chemotherapy, and show that blocking the proteins along with chemotherapy eliminate human leukemia in mouse models.
Reporting results March 20 in Nature Medicine, researchers at Cincinnati Children's Hospital Medical Center suggest that blocking the signaling proteins c-Fos and Dusp1 as part of combination therapy might cure several types of kinase-driven, treatment-resistant leukemia and solid tumor cancers.
These include acute myeloid leukemia (AML) fueled by the gene FLT3, lung cancers fueled by genes EGFR and PDGFR, HER2-driven breast cancers, and BCR-ABL-fueled chronic myeloid leukemia (CML), according to Mohammad Azam, PhD, lead investigator and a member of the Division of Experimental Hematology and Cancer Biology.
"We think that within the next five years our data will change the way people think about cancer development and targeted therapy," Azam says. "This study identifies a potential Achilles heel of kinase-driven cancers and what we propose is intended to be curative, not just treatment."
The weak spot is a common point of passage in cells (a signaling node) that appears to be required to generate cancer cells in both leukemia and solid tumors. The node is formed by the signaling proteins c-Fos and Dusp1, according to study authors. The researchers identified c-Fos and Dusp1 by conducting global gene expression analysis of mouse leukemia cells and human chronic myeloid leukemia (CML) cells donated by patients.
CML is a blood cancer driven by an enzyme called tyrosine kinase, which is formed by the fusion gene BCR-ABL. This fusion gene is the product of translocated chromosomes involving genes BCR (chromosome 22) and ABL (chromosome 9). Analysis of human CML cells revealed extremely high levels of c-FOS and DUSP1 in BCR-ABL-positive chemotherapy resistant cells.
Cancer sleeper cells
Cancer cells often become addicted to the mutated gene that causes them, such as BCR-ABL in kinase-driven chronic myeloid leukemia. Most chemotherapies work by blocking molecular pathways affected by the gene to shut down the disease process. In the case of CML, a chemotherapy called imatinib is used to block tyrosine kinase, which initially stops the disease. Unfortunately the therapeutic benefit is temporary and the leukemia comes back.
Azam and colleagues show in their CML models that signaling from tyrosine kinase - and growth factor proteins that support cell expansion (like interleukins IL3, IL6, etc.) - converge to dramatically elevate c-Fos and Dusp1 levels in the cancer cells.
Working together these molecules maintain the survival of cancer stem cells and minimal residual disease. The dormant cells wait around under the radar screen to rekindle the disease by acquiring additional genetic mutations after initially effective chemotherapy.
Azam says Dusp1 and c-Fos support the survival of cancer stem cells by increasing the toxic threshold needed to kill them. This means conventional imatinib chemotherapy will not eliminate the residual disease stem cells. Doctors can't just increase the dose of chemotherapy because it doesn't target the Dusp1 and c-Fos proteins that regulate toxic threshold.
Targeting c-Fos and Dusp1
After identifying c-Fos and Dusp1, the authors tested different treatment combinations on mouse models of CML, human CML cells, and mice transplanted with human leukemia cells. They also tested treatments on B-cell acute lymphoblastic leukemia (B-ALL).
The treatment combinations included: 1) solo therapy with just the tyrosine kinase inhibitor, imatinib; 2) solo treatment with just inhibitors of c-Fos and Dusp1; 3) treatment with all three combined - imatinib along with molecular inhibitors of c-Fos and Dusp1.
As suspected, treatment with imatinib alone initially stopped CML progression but the leukemia relapsed with the continued presence of residual disease cells. Treatment with c-Fos and Dusp1 inhibitors alone significantly slowed CML progression and prolonged survival in a majority of mice but wasn't curative. Treatment for one month with c-Fos/Dusp1 inhibitors and imatinib cured 90 percent of mice with CML, with no signs of residual disease cells.
Azam and his colleagues also point to an interesting finding involving solo treatment with just the deletion of c-Fos and Dusp1. This eliminated expression of the signaling proteins and was sufficient to block B-ALL development, eradicating the disease in mouse models.
Next steps
The authors stress that because the study was conducted in laboratory mouse models, additional research is needed before the therapeutic strategy can be tested in clinical trials.
They are following up the current study by testing c-Fos and Dusp1as treatment targets for different kinase-fueled cancers, including certain types of lung cancer, breast cancers and acute forms of leukemia.
More information: Targeting c-FOS and DUSP1 abrogates intrinsic resistance to tyrosine-kinase inhibitor therapy in BCR-ABL-induced leukemia, Nature Medicine, nature.com/articles/doi:10.1038/nm.4310














