European countries restrict access to life-saving treatment for hepatitis C
Data presented today demonstrate that there are considerable restrictions in the reimbursement of direct-acting antiviral (DAA) therapy across European countries, particularly with respect to the severity of liver fibrosis (scarring of the liver) and prescribing by specialists. The study, presented at The International Liver Congress 2017 in Amsterdam, The Netherlands, showed that there was evidence that some countries were not following the most recent European HCV treatment guidelines, published by the European Association for the Study of the Liver (EASL) in 2016.1
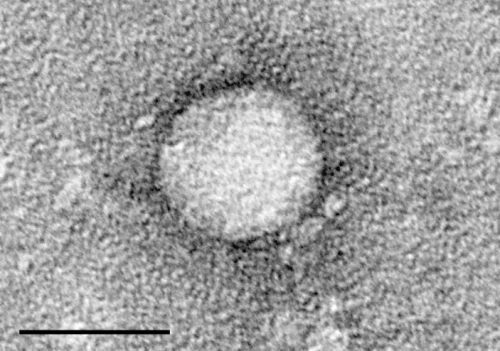
HCV is one of the most widespread transmissible diseases.2 It can cause both acute and chronic infection, with about 55-85% HCV-infected individuals developing chronic infection.3 HCV is a leading cause of chronic liver disease, end-stage cirrhosis and liver cancer.4 It is estimated to infect over 71 million people worldwide, of whom 784,000 die each year.5,6 Until the approval of the DAAs, HCV was treated with pegylated interferon and ribavirin, which caused serious adverse effects in more than 80% of patients, and fewer than 50% were able to finish the course of therapy.2 These new drugs have revolutionised treatment and mean that HCV is now curable, with a cure rate of 95% or higher.7 Although the DAAs are highly effective, they are expensive and unaffordable if prescribed for all patients.1 Most countries therefore limit access to these drugs.
"The availability of simple, tolerable DAA-based therapies for HCV with high cure rates is one of the greatest clinical advances in recent decades," said Ms Alison Marshall, PhD candidate, Kirby Institute, UNSW Sydney, Australia, and author of the study. "While all European countries included in our study reimbursed some form of DAA treatment, there was restricted access based on fibrosis stage, substance use, and type of prescriber, meaning that some patients are encountering considerable barriers to the life-saving treatment they need. In particular, restricting DAA prescribing to specialists is a major impediment to ensuring broad access to HCV therapy. These findings have important implications for health policy makers and the delivery of health services across Europe."
Information from online reimbursement documents for EU/EEA countries (including England, Northern Ireland, Scotland, and Wales as separate jurisdictions) and Switzerland were reviewed from November 2016 to March 2017. Primary outcomes were reimbursement restrictions based on the stage of fibrosis, drug or alcohol use, type of prescriber (e.g. specialists), and HIV-HCV co-infection.
The European countries with complete data (34/35) all reimbursed DAAs. The most common DAAs reimbursed were ombitasvir/paritaprevir/ritonavir ± dasabuvir ± ribavirin (97%) and sofosbuvir/ledipasvir ± ribavirin (88%). For treatment naïve patients, 38% (n=13) of countries required evidence of at least moderate fibrosis (?F2)8 before DAAs were prescribed, nearly a quarter (24%, n=8) required at least severe fibrosis (?F3),8 over a quarter (26%, n=9) had no fibrosis stage restrictions, and 9% (n=3) had an additional requirement, such as genotype of HCV. In this study, 76% (n=26) of countries had no drug or alcohol use restriction, though almost one-fifth (n=6) had a drug or alcohol use limitation (e.g. abstinence required prior to treatment with DAAs). Overall, 94% (n=32) of countries had no additional restrictions for HIV-HCV co-infection, and in fact, 24% (n=8) of countries gave priority status to HIV-HCV co-infected people with fewer restrictions than for HCV mono-infected people. Further, 94% (n=32) of countries required specialists to prescribe DAA therapy.
"Restrictions to DAA access for Hepatitis C across Europe are widespread and conflicting with the EASL Clinical Practice Guidelines, thus preventing many patients from being treated. Restrictions are the consequence of current drug prices, calling for revised strategies to make these treatments available to all in need," said Prof Francesco Negro, Divisions of Gastroenterology and Hepatology of Clinical Pathology, University Hospital of Geneva, Switzerland and EASL Governing Board Member.
More information: Abstract: Restrictions for reimbursement of interferon-free direct-acting antiviral therapies for HCV infection in Europe (LBP-505), The International Liver Congress 2017.
References:
1 European Association for the Study of the Liver. EASL recommendations on treatment of hepatitis C 2016. J Hepatol. 2017;66(1):153-94.
2 World Health Organization. Access to new medicines in Europe: technical review of policy initiatives and opportunities for collaboration and research. March 2015. Available from: apps.who.int/medicinedocs/docu … 21793en/s21793en.pdf. Last accessed: April 2017.
3 World Health Organization. Hepatitis C in the WHO European Region Fact Sheet. July 2015. Available from: www.euro.who.int/__data/assets … et-en-hep-c.pdf?ua=1. Last accessed: April 2017.
4 Mühlberger N, et al. HCV-related burden of disease in Europe: a systematic assessment of incidence, prevalence, morbidity, and mortality. BMC Public Health. 2009;9:34.
5 The Polaris Observatory HCV Collaborators. Global prevalence and genotype distribution of hepatitis C virus infection in 2015: a modelling study. Lancet Gastroenterology and Hepatology. 2016;2(3):161-176.
6 Stanaway J, et al. The global burden of viral hepatitis from 1990 to 2013: findings from the Global Burden of Disease Study 2013. Lancet. 2016;388(10049):1081-1088.
7 Liang T, Ghany M. Current and future therapies for hepatitis C virus infection. N Engl Med. 2013;369(7):679-680.
8 Goodman ZD. Grading and staging systems for inflammation and fibrosis in chronic liver disease. J Hepatol. 2007;47:598-607.















