Do meds like Remifemin really ease hot flushes and night sweats in menopausal women?

If you see a female friend or colleague sitting in front of a desk fan in winter while everyone else is shivering in sweaters, chances are she is having a hot flush, courtesy of the menopause.
Hot flushes and night sweats are the most common symptoms of the female reproductive milestone. The menopause is often blamed for a host of other symptoms such as insomnia, joint pains, depression and mood swings, vaginal dryness and difficulty concentrating.
Hot flushes can last for years and be debilitating, and conventional treatments such as hormone replacement therapy (HRT) and antidepressants come with risks. HRT increases the chance of developing potentially deadly clots in the leg veins; a small increase in breast cancer risk has also been reported.
Because of these risks, women may turn to herbal products that are purportedly safer and have fewer side effects. A native American root called black cohosh (Actaea racemosa) is included in many such treatments used for hot flushes.
The root has a long history of use in Europe and became popular around the world after receiving German approval as a non-prescription drug for hot flushes in 2000. In Australia, it is sold in various formulations and promoted as:
a safe and natural way to help reduce symptoms such as hot flashes and night sweats.
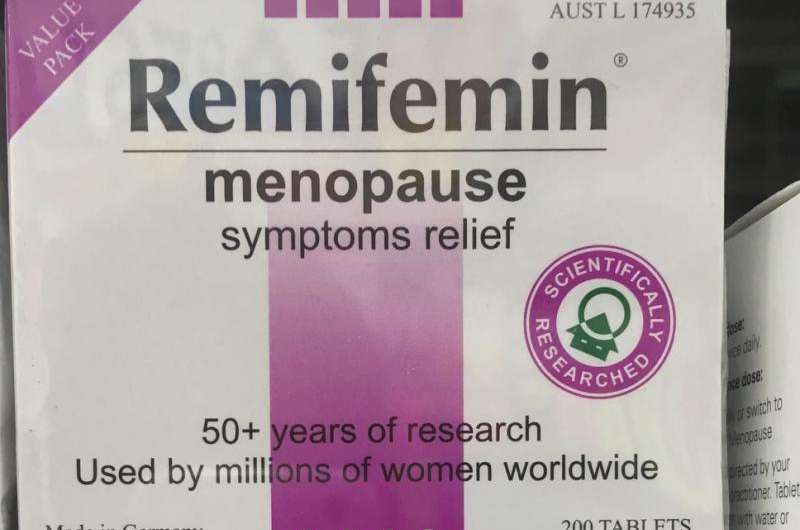
Apart from menopausal symptoms, black cohosh is also used to treat arthritis and premenstrual syndrome. It is the main ingredient in the product sold in many pharmacies called Remifemin, which claims to be "one of Germany's foremost herbal products and is used in more than 25 countries." But does this herb live up to the marketing?
How is black cohosh used?
Native Americans didn't only use black cohosh to treat female reproductive problems such as "menstrual irregularities", they also used it for pain, fever and cough.
The root is most commonly sold as an extract in capsule form, but can also be taken as a liquid tincture or tea. Commercial formulations vary in dose and form.
Although the root and rhizome (the stalk of the root) of the black cohosh plant contain a number of active ingredients, its mechanism of action when it comes to menopausal symptoms remains unclear.
It may work by affecting chemical compounds related to female hormone levels (such as oestrogen), but evidence on this is still vague.
Does it work?
The evidence for whether or not black cohosh eases hot flushes is unfortunately inconclusive. Some studies show it works, while others don't. It is important to note that there is often a high placebo effect with hot flush treatments.
In 2012, a Cochrane review pulled together results from 16 studies evaluating the effectiveness of black cohosh. There was no difference in the number of weekly, or daily, hot flushes between women who received black cohosh and women who received a placebo.
There was also a similar side effect profile between placebo and treatment. However, only three trials were suitable for the side effect analysis.
The Cochrane authors were unable to make a definitive conclusion about how effective black cohosh was for menopausal symptoms for a number of reasons. These included design flaws in many of the trials evaluated, differences in the types of herbal extract used, and variation in the way symptoms were reported.
Some trials did not report a dose for black cohosh, while the duration of treatment ranged from eight weeks to 12 months.
A more recent and well-designed trial of 84 menopausal women in Iran showed those allocated to take a standardised extract of black cohosh ("Cimifugol") reported an 82% reduction in daily hot flushes, compared to 24% in the placebo group after eight weeks.
But when these results were combined with those from previous similar trials in a 2016 meta-analysis, no difference between groups was found.
A subsequent 2015 trial in 54 Thai women did not find black cohosh to be effective for menopausal symptoms. However, another small trial reported both subjective and objective improvements in sleep disturbance.

Is it safe?
A 2008 review was conducted by a US dietary supplements expert committee after around 30 reports of liver failure in patients from the European Union, Canada and Australia (one death was reported), were "potentially associated" with black cohosh. It found the liver toxicity was possibly (but not probably) linked to black cohosh.
This means there is a very small risk of liver failure, which is potentially fatal, for those taking black cohosh. Women should seek urgent medical attention if they develop abdominal pain, fatigue, have dark urine or jaundice.
It should be noted clinical trials have not reported a link between black cohosh and liver failure, and that the association may be due to other factors affecting liver health (such as alcohol consumption) or lack of quality control in commercial preparations. That is to say, black cohosh has not been proven to cause liver failure.
Also, overall side effects from black cohosh are considered rare (one in 14,000 to one in 100,000).
Other remedies
In 2015, a large Australian survey of women aged 40 to 65 reported 13% of survey respondents took a complementary medicine for hot flushes. Phytoestrogens (such as red clover and soy isoflavones) were the most popular. There is evidence these may reduce the number of hot flushes by a modest 1.3 flushes a day.
Phytoestrogens are considered a relatively safe supplement. Yoga, mindfulness meditation and cognitive behavioural therapies also show promise. Although black cohosh was the fourth most popular complementary therapy used by survey respondents, it was only used by 1.5% of women.
Acupuncture was initially thought to be effective for hot flushes, but a large 2016 Australian study reported no difference between real and sham acupuncture.
While results on whether black cohosh improves menopausal symptoms are mixed, this is not to say we know for sure black cohosh doesn't work. Rather, the inconclusive findings reflect some of the problems with complementary medicine research, including the use of varying doses and formulations leading to difficulties making conclusions.
Women who use black cohosh should be aware of these uncertainties and of the small risk of liver failure that has been reported.
This article was originally published on The Conversation. Read the original article.![]()
















