May 10, 2017 report
Transplanting rat testes to secondary rat's neck to preserve spermatogenesis
(Medical Xpress)—A team of researchers with members from Tokyo Medical University and Aichi Medical University, both in Japan, has tested the feasibility of removing testes from one rat and surgically implanting them into the neck of another rat to preserve spermatogenesis for the first rat. In their paper uploaded to the open access site PLOS ONE the group describes how the procedure worked, and compared it to attempts to transplant testes into a host groin.
When men or boys are diagnosed with certain types of cancers, particularly leukemia, or if cancer is detected in one or more testicles, they are quite often encouraged to have samples of their semen frozen for later use, because some treatments can leave them permanently sterile. With younger, prepubertal patients, this is not an option, which means they will never be able to sire offspring.
To get around this problem, scientists have been investigating the possibility of removing the parts of the testicles that produce sperm and implanting them into another person—such as a brother or a father. This is possible because testes have properties that prevent the immune system from attacking them. If the transplanted testes continue to produce sperm, they can be harvested at a later date, or even better, be returned to the original patient after completion of cancer treatment. Prior research has found that because of the physical structure of the parts inside of the testicular sack, moving parts of a testicle from one rat testicular sack to another is particularly difficult. That has led some researchers to consider putting them elsewhere inside of a host. In this case, the researchers removed testes from several rats and placed them inside the necks of other rats to test the feasibility of such an approach.
The researchers report that they conducted the procedure on 12 rats and, for comparison, also implanted testes into the testicular sacks of several host rats. They further report a 100 percent success rate with the neck procedures but just 71 percent with sack-to-sack transfers. They also report that the neck transfer procedures took on average 60 minutes, while the sack-to-sack procedures took on average 154 minutes. The researchers suggest their findings indicate that neck implantations appear to be a better option thus far. More testing is required to learn about the survival rates of testes in the neck and how long they will continue to produce sperm.
More information: Kai Yi et al. Development of heterotopic transplantation of the testis with the epididymis to evaluate an aspect of testicular immunology in rats, PLOS ONE (2017). DOI: 10.1371/journal.pone.0177067
Abstract
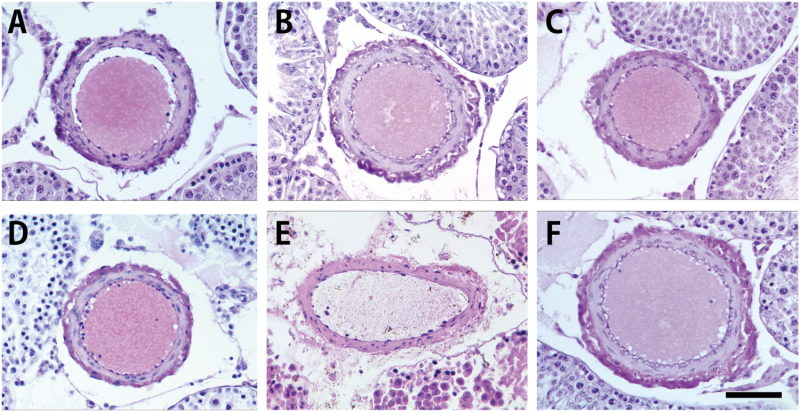
Transplantation of testicular cells and tissues has been studied for the investigation of immunology of the testis, which is an immunologically privileged organ. However, reports of transplant of the testis at organ level have been extremely limited because of technical difficulties of the orthotopic testis transplantation (OTT) in experimental animals. In the present study, we developed a new and simple model of the heterotopic testis transplantation (HTT), which is donor testis transplantation into the cervical region of recipients, in a syngeneic model in rats [donor Lewis (LEW) graft to LEW recipient]. The duration of HTT was significantly shorter and success rate higher than that of OTT. To histologically evaluate HTT, the local immune responses were compared among the syngeneic model, an acute rejection allogeneic model [donor Augustus Copenhagen Irish (ACI) graft to LEW recipient] and a chronic rejection allogeneic model (donor F344 graft to LEW recipient) at postoperative day 3. We found that allogeneic ACI grafts resulted in mild and not severe orchitic lesions, whereas immune responses of allogeneic F344 grafts seemed intact and were not significantly different from those of syngeneic LEW grafts. These results suggest that our new operative procedure will be useful in future for the investigation of the testicular immunology.
© 2017 Medical Xpress




















