New research shows indigenous peoples are much more likely to be infected by hepatitis B and/or C
A new meta-analysis of global hepatitis data—presented at this year's World Indigenous Peoples' Conference on Viral Hepatitis in Anchorage, Alaska, USA (8-9 August)—shows that Indigenous Peoples are up to 10 times more likely to be infected by viral hepatitis than the general population in their respective countries. The analysis is presented by Dr Homie Razavi and Devin Razavi-Shearer, The Polaris Observatory, Lafayette, CO, USA.
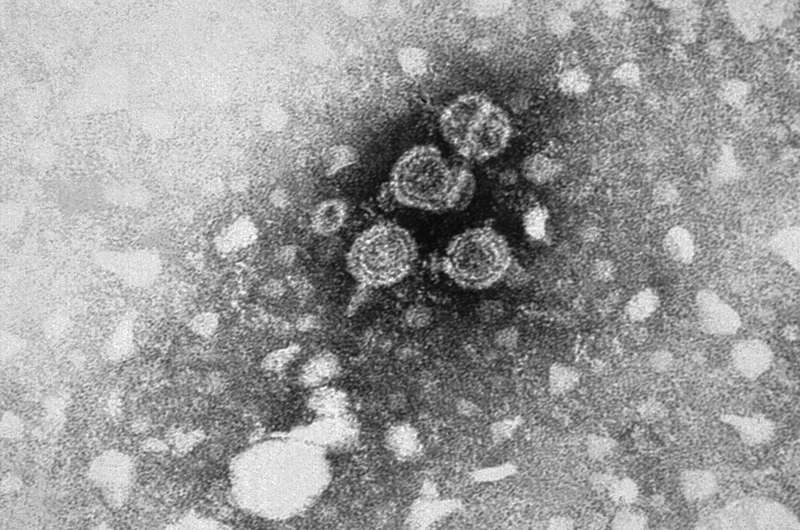
Both hepatitis B and hepatitis C are viral infections, which, if left untreated, can cause serious liver damage, liver cancer, and ultimately death. Both can be transmitted through contact with the blood of an infected person, sexual transmission, injection drug use, unsafe medical procedures and tattooing where equipment has not been sterilised. Hepatitis B is also commonly sexually transmitted.. For hepatitis C, people who received a blood transfusion before 1992 when universal blood screening practices were introduced in most high-income countries, are also at risk.
An estimated 71 million people worldwide have chronic hepatitis C infection; for hepatitis B the numbers are higher at 257 million. Most people with hepatitis B virus are adults infected before the hepatitis B vaccine became widely available.
In this new research, the authors reviewed prevalence of both viruses in the Indigenous Peoples and general populations of North America, South America, Australia, and New Zealand. For hepatitis C, data that could be extrapolated to the general population was found for 11 countries and included 23 specific Indigenous Peoples and nations as well as 12 more broad groupings, covering the period from 1991 onwards.
The data showed that, compared to general populations in their countries:
- Hepatitis C rates among Aboriginal and Torres Straight Islanders are 3 times higher
- In Canada, the Inuit and Métis First Nations Canadians also have rates 3 times higher
- In New Zealand, the data were insufficient to produce reliable estimates
- In the continental USA, American Indian tribal citizens overall had rates 2.5 times higher
- In Alaska, there was no statistically significant difference in the rate of hepatitis C in Alaskan natives.
The authors say: "The higher prevalence of anti-HCV observed in Indigenous Peoples and nations can be the result of disproportionately high rates of poverty, injection drug use, and incarceration in Iindigenous populationsPopulations. This, in combination with the lack of access to healthcare and prevention measures, greatly increases the risk and thus prevalence of hepatitis C."
For hepatitis B, prevalence was reviewed among Indigenous Peoples and nations of North America, South America, Australia, and New Zealand. Data that is suitable for extrapolation was found for 13 countries and included 106 specific Indigenous Peoples and nations as well as 22 more broad groupings.
The data showed that, compared with their respective general populations:
- Aboriginal and Torres Straight Islanders in Australia were 4 times more likely to have hepatitis B infection
- Maori and Pacific Islander populations in New Zealand had double the rates of hepatitis B
- Canadian First Nations Inuit and Metis peoples had an even higher disparity, with hepatitis B rates five times higher
While USA Alaskan native populations had rates of hepatitis B 10 times that of general population (the largest disparity found), the studies included did not take into account universal hepatitis B vaccination in that state that has almost wiped out new infections in young people, and this will have brought down overall hepatitis B prevalence in recent years
The authors add that today, hepatitis B vaccination rates are similar among Indigenous and non-Indigenous young people across the USA.
The authors say: "The distribution of the prevalence of hepatitis B varies greatly among different indigenous Peoples and nations, and in some Indigenous Peoples of the Amazon it has been reported that the prevalence can even vary drastically by village. The disparities in access to healthcare, prevention, and treatment in particular have continued to reinforce the prevalence, morbidity and mortality disparities that are seen."
Raquel Peck, Chief Executive of the World Hepatitis Alliance, London, UK, said: "These data confirm that Indigenous Peoples worldwide are bearing a disproportionately high burden of hepatitis B, hepatitis C, or both. More must be done to ensure that Indigenous Peoples everywhere are at the heart of hepatitis treatment and prevention programs."



















