Neuroscientists identify genetic changes in microglia in a mouse model of neurodegeneration and Alzheimer's disease
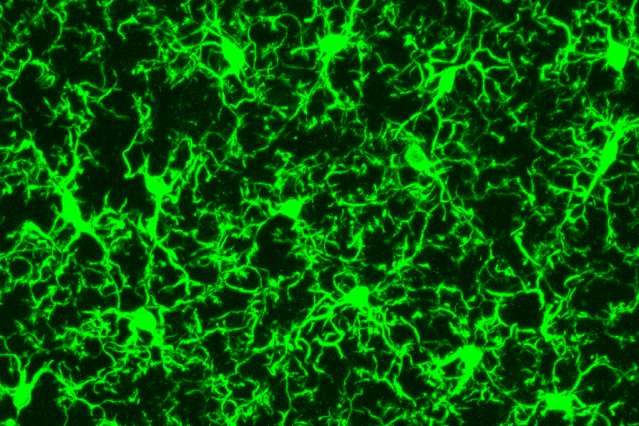
Microglia, immune cells that act as the central nervous system's damage sensors, have recently been implicated in Alzheimer's disease.
The cells, a type of macrophage that clear away dead cells from the brain and help to maintain healthy neuronal wiring, were found to be entangled with toxic amyloid beta plaques in tissue taken from those suffering from the disease.
Researchers had previously believed that the cells help to protect the brain from neurodegeneration by digesting the amyloid plaques, but it now appears the immune system may play a role in the progression of Alzheimer's disease.
However, exactly what this role is, and how microglia are transformed from their protective state in healthy brains into a harmful state as the disease progresses, remains unclear.
To better understand microglia and how they respond in this way, a team led by MIT Professor Li-Huei Tsai, director of MIT's Picower Institute for Learning and Memory, used single-cell RNA sequencing to study individual microglia cells. The research, published in the journal Cell Reports, represents the first time individual microglia have been studied in this way, according to Tsai.
"Right now, microglia are really in the spotlight for a number of neuro-system diseases, including Alzheimer's, and also schizophrenia," Tsai says. "However, there are still a lot of very basic things that we don't know about microglia, such as whether cells in the healthy and diseased brain are all the same, or whether there are different groups, and how they become more inflammatory in the diseased state."
The researchers used single-cell RNA sequencing to measure active gene expression in individual microglia cells in a mouse model of Alzheimer's disease previously developed by Tsai's lab. The mice were engineered so that the gene for a protein called p25 can be overstimulated in the brain, prompting the mice to develop symptoms very similar to those found in Alzheimer's disease in humans.
The researchers used the technique to study what happens to microglia cells at various points in the progression of neurodegeneration. They measured the cells just before the induction of p25, and then one week, two weeks and six weeks after p25 induction, according to first author Hansruedi Mathys, a postdoc at the Picower Institute.
"This allowed us to follow how microglia respond to the progression of the disease, and the worsening conditions in the mouse brain," Mathys says.
Surprisingly, they found that just one week after p25 induction, the microglia had already begun to respond to the threat by proliferating more than cells in the control mice.
"This means that the microglia must be able to sense some sort of perturbation in the mouse brain at a very early time point," Mathys says.
They then looked at the response from the microglia at two and six weeks after p25 induction, and found that the cells had stopped proliferating, and had instead begun to mount a pronounced immune response. Indeed, they found that hundreds of genes relating to an immune response were activated at these later stages of disease progression.
"The microglia initially transition from a resting state into a proliferation state, after which they transition again into a mainly inflammatory state, with very high expression of genes with a very specific immune system function," Tsai says.
They also discovered distinct groups of microglia, which were found only in the later stages of neurodegeneration. One type of microglia was found to only express interferon response genes, for example, while another only expressed histocompatibility complex class II (MHC) genes.
To find out if these distinct types of microglia overlap geographically, the researchers then performed a technique known as immunostaining to investigate where the populations of cells were distributed in the mouse brain. They stained different sections of the mouse hippocampus with antibodies that recognise particular gene products.
They found that the different types of microglia have very different distribution patterns.
The study is the first to combine single-cell RNA sequencing in microglia with an analysis of gene expression in an inducible model of neurodegeneration, says Tony Wyss-Coray, a professor of neurology and neurological sciences at Stanford University, who was not involved in the research.
"I find it particularly exciting that cells transition through different phases, seemingly following different gene expression programs," Wyss-Coray says. "This confirms the suspicion that there is a lot of cellular heterogeneity in microglial response to damage, but this paper actually shows this for the first time in a temporal fashion."
It is also intriguing that microglia show such a strong interferon and MHC class II response, as if reacting to viral infection, he says. "If this response turns out to be key to subsequent neuronal damage, it could provide a novel target for intervention."
The researchers now hope to investigate whether the genes that are expressed by the microglia, including interferon response genes, might offer a potential new target for drug discovery.
"We're planning to interfere with type I interferon signalling in this mouse model, to see if it has any beneficial effect on cognition, or disease pathology," says Mathys.
More information: Hansruedi Mathys et al. Temporal Tracking of Microglia Activation in Neurodegeneration at Single-Cell Resolution, Cell Reports (2017). DOI: 10.1016/j.celrep.2017.09.039
This story is republished courtesy of MIT News (web.mit.edu/newsoffice/), a popular site that covers news about MIT research, innovation and teaching.


















