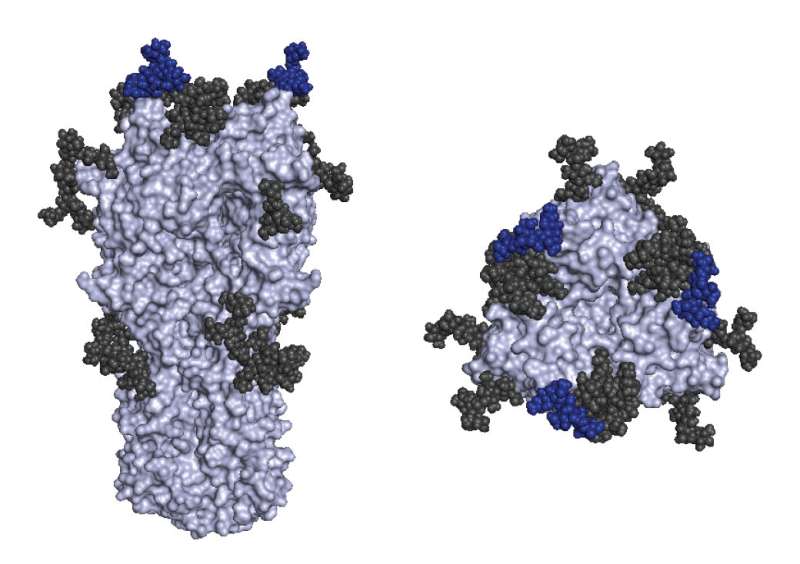
The major flu vaccine antigen, hemagglutinin, is shown. Colored in dark blue is a region of the vaccine that differs between the current egg-grown H3N2 vaccine strain and circulating H3N2 viral strains. Credit: Zost et al, PNAS, 2017
The low efficacy of last year's influenza vaccine can be attributed to a mutation in the H3N2 strain of the virus, a new study reports. Due to the mutation, most people receiving the egg-grown vaccine did not have immunity against H3N2 viruses that circulated last year, leaving the vaccine with only 20 to 30 percent effectiveness. Scott Hensley, PhD, an associate professor of Microbiology, in the Perelman School of Medicine at the University of Pennsylvania, describes his team's findings in the Proceedings of the National Academy of Sciences this week.
"Our experiments suggest that influenza virus antigens grown in systems other than eggs are more likely to elicit protective antibody responses against H3N2 viruses that are currently circulating," Hensley said. "The 2017 vaccine that people are getting now has the same H3N2 strain as the 2016 vaccine, so this could be another difficult year if this season is dominated by H3N2 viruses again."
Flu vaccines work by priming the immune system with purified proteins from the outer layer of killed flu viruses. This induces immune cells to make antibodies that stop foreign invaders from infecting cells, readying them to attack flu viruses when the body sees them again. Most flu vaccine proteins are purified from a virus grown in chicken eggs, although a small fraction of flu vaccine proteins are produced in systems that do not involve eggs.
During the 2014-2015 flu season, a strain of the H3N2 virus with a different outer layer protein emerged and this version of H3N2 remains prevalent today. The 2016-2017 seasonal flu vaccine was updated to include the new version of this protein; however, Hensley's lab found that the egg-grown version of this protein acquired a new mutation. "Current H3N2 viruses do not grow well in chicken eggs, and it is impossible to grow these viruses in eggs without adaptive mutations," Hensley said.
The team showed that antibodies elicited in ferrets and humans exposed to the egg-produced 2016-2017 strain did a poor job of neutralizing H3N2 viruses that circulated last year. However, antibodies elicited in ferrets infected with the current circulating H3N2 viral strain (that contains the new protein) and humans vaccinated with a H3N2 vaccine produced in a non-egg system were able to effectively recognize and neutralize the new H3N2 virus.
"Our data suggest that we should invest in new technologies that allow us to ramp up production of influenza vaccines that are not reliant on eggs," Hensley said. "In the meantime, everyone should continue to get their annual flu vaccine. Some protection against H3N2 viruses is better than nothing and other components of the vaccine, like H1N1 and influenza B, will likely provide excellent protection this year."
More information: Seth J. Zost el al., "Contemporary H3N2 influenza viruses have a glycosylation site that alters binding of antibodies elicited by egg-adapted vaccine strains," PNAS (2017). www.pnas.org/cgi/doi/10.1073/pnas.1712377114
Journal information: Proceedings of the National Academy of Sciences