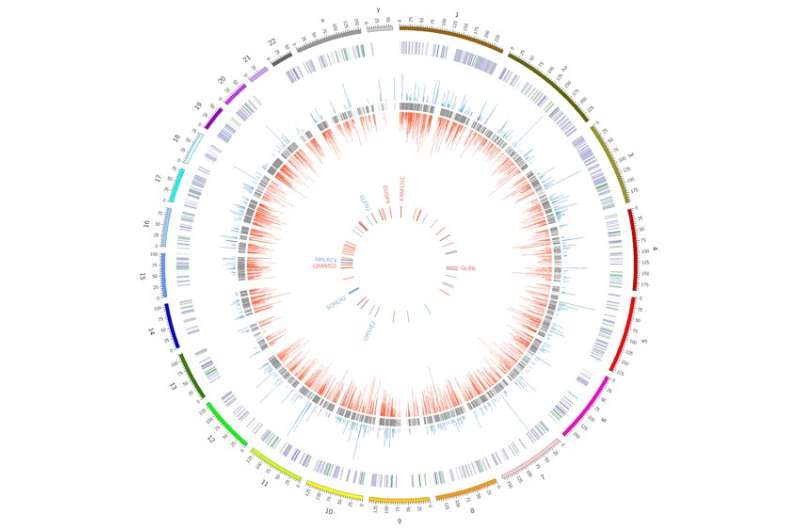
This plot represents a circularized version of the human genome. Each subsequent inner ring represents novel findings in the study relevant to disease. Credit: Christopher McNair, Thomas Jefferson University
The retinoblastoma (RB) susceptibility gene was the first gatekeeper gene discovered for cancer. When it was removed, or damaged, cancers thrived. Over the years, researchers discovered many methods to experimentally remove the RB gene in order to study it, but just how the gene's loss made cancers more aggressive in patients was poorly understood. By studying patient samples, researchers at Thomas Jefferson University and colleagues found how one type of RB removal, but not another, caused large-scale genetic changes that could make cancer both resistant to treatment and more likely to spread.
"RB loss causes a major reprogramming of gene expression, allowing induction of pathways that promote features that induce characteristics of lethal disease," said senior author Karen Knudsen, PhD, Director of the Sidney Kimmel Cancer Center (SKCC) at Thomas Jefferson University. The study is the first to identify the molecular consequences of RB loss and illustrate the clinical relevance of RB-loss-induced transcriptional rewiring.
The work involved a multinational collaboration between SKCC investigators at Thomas Jefferson University and other US-based laboratories, as well as clinical and basic science researchers in the UK, Italy, Belgium, Finland and Sweden. It was published online December 4th in The Journal of Clinical Investigation.
Spearheaded by first author Christopher McNair, PhD, a graduate student in the laboratory of Dr. Knudsen, the study undertook an extensive analysis of tumor samples and cell-free DNA samples from patients with advanced, lethal-stage prostate cancer. Although there are several ways to remove RB from the cellular machinery, the group found that complete loss, rather than inactivation, of the RB gene was associated with changes in gene-networks closely linked to aggressive disease. Surprisingly, the cancer-promoting program that RB-loss unleashed was distinct from the cell-cycle control genes that RB is best known for controlling.
The new findings hold great promise for further clinical development and application. First, the research demonstrates that RB status can be tracked using cell-free DNA samples, an approach referred to as "liquid biopsy", in prostate cancer patient samples. This method will facilitate the analysis of patient tumors and the selection of the most appropriate therapy based on the individualized features of each patient's cancer subtype. Multiple clinical trials are now underway in Philadelphia that will determine the impact of RB status as a means to guide more precise cancer therapy. "Unlike breast cancer, all prostate cancers are currently treated in an identical fashion. This discovery, and the clinical trials we have underway, suggest that RB status might be used as means to stratify patients into more effective treatment regimens," said William Kevin Kelly, leader of the Prostate Cancer Program at SKCC.
More information: Christopher McNair et al, Differential impact of RB status on E2F1 reprogramming in human cancer, Journal of Clinical Investigation (2017). DOI: 10.1172/JCI93566
Journal information: Journal of Clinical Investigation
Provided by Thomas Jefferson University