New technique could reveal immunotherapy targets, study finds
Researchers at the Stanford University School of Medicine and their colleagues have developed a way to pinpoint potential targets for cancer therapies that rely on the body's immune system.
Those targets are molecules called antigens, which appear on the surface of tumor cells and other malignant or damaged cells. Antigens are cumbersome to identify but critical to developing cancer immunotherapies, a type of treatment in which the host's own immune system is trained to seek out and fight harmful or mutated cells. And while cancer vaccines are still largely a thing of the future, new antigens are key to nudging progress forward.
The researchers exploited years of structural and protein engineering studies by the laboratory of Christopher Garcia, PhD, professor of molecular and cellular physiology and of structural biology, to better understand how the immune system "sees" antigens. Based on this knowledge, they developed a technique to identify them. What's more, the technique could serve to identify potential antigens relevant to other immunotherapies, such as those that combat autoimmune or infectious diseases.
A paper describing the work will be published online Dec. 21 in Cell. Stanford graduate student Marvin Gee and postdoctoral scholar Arnold Han, MD, PhD, share lead authorship of the paper. Garcia, who holds the Younger Family Professorship, is the senior author.
"The whole foundation of immunotherapy depends on immune cells recognizing specific antigens on tumor cells. That's the basis of the actual killing event—where the rubber hits the road," Garcia said. "But currently we know very few tumor antigens, and there's just been no good way of discovering them." Here, he said, is where he sees potential for the new biochemical screen to expedite the identification process.
A game of odds
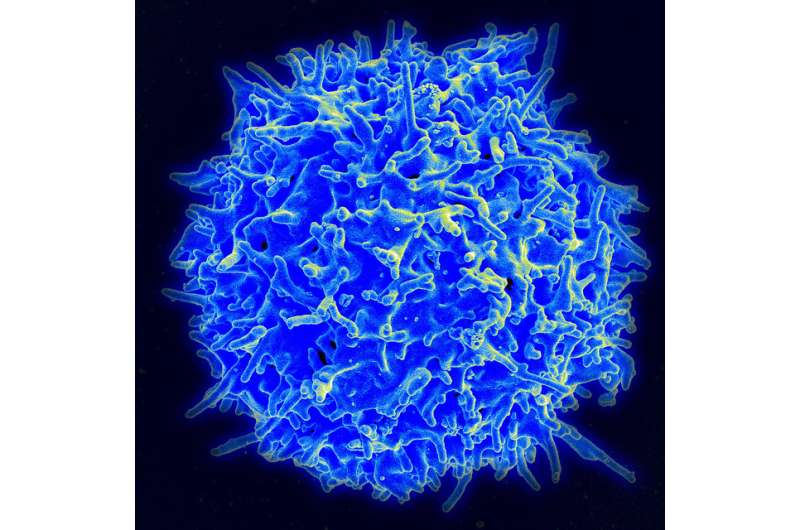
A type of immune cell known as a T cell patrols the body for foreign invaders or mutated cells poised to cause harm. On their surface, T cells have receptors that bind to one or more specific antigens of a tumor or other harmful cell. When a receptor finds its match, the antigen acts as the T cell's molecular directive to infiltrate and kill the unhealthy cell. But because matched receptor-antigen pairs are difficult to come by experimentally, many receptors remain unidentified. They're called orphan receptors.
"This screen is a completely unbiased way of taking a random T cell receptor that's infiltrated a tumor and interrogating it to find out exactly what antigen it is actually seeing," said Garcia, who is a Howard Hughes Medical Institute investigator.
The screen he and his colleagues devised pulls data from two resources: orphan T cell receptors found on colon cancer tumors, and a hefty repository of antigen sequences of white blood cells. Using yeast as a vehicle, the team scanned some 400 million of these antigen sequences, all possible matches to 20 orphan receptors derived from the colon cancer tissue samples. Four of the 20 receptors found matches.
The somewhat modest ratio is a product of chance. The receptors are restricted by genotype, and will only bind to antigens of a matching genotype. Between that and the enormous variability of possible antigens, pegging a receptor-antigen match is "a bit like winning the lottery," Garcia said. "The key to increasing the odds is to increase the throughput of the experiments, kind of like putting more coins into the slot machine."
What's in the screen, and what's getting screened, Garcia explained, are mimics of the original receptors and antigens—accurate, but not 100 percent identical. So, after the initial screen, the four receptors that bound antigens were then sequenced and run through an algorithm, which ultimately figured out the correct corresponding identity of the human antigen. With this technique, the team unambiguously identified two human antigens of the four receptors that found matches in the yeast-based library, and they're currently in the process of identifying a third one.
Neo versus self
There's an ongoing debate, Garcia said, about the most important types of antigens that T cells "see" and attack in tumors. One currently popular notion is that T cell receptors react with neoantigens, or antigens that are mutated or uniquely part of a cancer, rather than self-antigens, which both cancerous and healthy cells can have in common. Unexpectedly, however, evidence from the new study suggests otherwise, as one of the two antigens was "self." In addition, the self-antigen turned out to be shared between two patients—a key to developing immunotherapies.
"It was a huge surprise to find that one of the antigens was a non-mutated, shared self-antigen, and the implications are that if you screen many more T cell receptors, you'll likely find a lot of shared antigens," Garcia said. "So in theory, you could have one immunotherapy that targets this antigen, and it'd be effective for multiple patients." But this, he said, brings us to the million-dollar question: How do we generate anti-tumor immunity against an antigen that is attached to both healthy and cancerous cells?
"Right now, we don't have an answer, but there are a lot of efforts going into that problem, and it's something that I'm very interested in," Garcia said. "It's a problem that we're going to have to solve because there are going to be a lot of tumor antigens that will be non-mutated, and so we have to figure out how to localize the attack to just the tumor, and not the rest of the host."
















