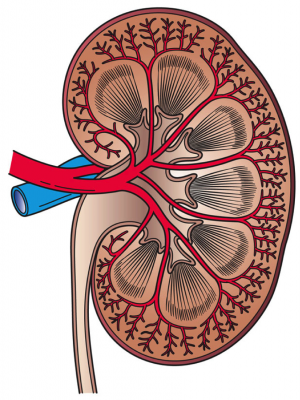
This image shows a cross section of a kidney. Credit: Holly Fischer/Wikipedia
Paulette McIlvena went to bed, at home, and woke up three weeks later, in hospital. She became severely ill due to complications from pancreatitis. While she was in a coma McIlvena underwent surgery and was put on dialysis as a temporary measure. Following those events in 2004, the pancreatitis cleared up, McIlvena's kidneys started working again, and she thought her kidney troubles were behind her.
Recently, however, she was diagnosed with chronic kidney disease related to her experience 13 years ago and is now being treated by UCalgary's Cumming School of Medicine physician-scientist Dr. Matthew James.
James says 12 per cent of people who are hospitalized will experience a kidney complication, despite being admitted for a different reason. Called acute kidney injury, for some, the problem can be as simple as not making as much urine; for others, like McIlvena, the kidneys stop functioning, for a time.
"There are a wide range of outcomes after someone experiences acute kidney injury. Many patients will have a good recovery and their kidney function will return to normal, but others can develop kidney failure afterward," says James.
Until recently, doctors had no way to know which patients were most at risk of long-term complications. Through research, James and his colleagues developed a risk assessment tool that can now be used in Alberta hospitals to guide subsequent care. "We don't want to miss the people who will have long-term kidney health problems," says James. "The tool allows us to identify people who need followup and tailor care specifically for them."
Kidney disease is considered a silent disease; you often don't know you're sick until you're into the late stages of the illness, where treatment means dialysis for life, or transplant.
The science behind the risk assessment tool
To design a tool that could hone in on whether acute kidney injury may progress to advanced chronic kidney disease, two groups of patients were studied. Over the course of 11 years, data from 9,973 Alberta patients was reviewed with six health measurements routinely taken: age, sex, urine protein levels, kidney function levels when admitted to hospital, kidney function levels throughout hospital stay, and kidney function levels when discharged.
Combined, these factors provided researchers with a framework with which to estimate a patient's risk level of developing advanced kidney disease over the next year. To confirm the approach, 2,761 patients from Ontario were assessed. The results validated the model. The study is published in the Journal of the American Medical Association.
The research team will evaluate the tool in clinical practice; they know the tool works and now they want to find out if using it can improve care and outcomes for patients. Patients with acute kidney injury in Calgary and Edmonton will be eligible to join the next study. If use of the tool results in better followup care and outcomes for patients after hospital discharge, then strategies to scale up its use across Canada could begin. The model could also be used in other countries down the road.
"We hope to improve the experiences for patients and tools available for health care providers, by providing them with personalized risk information, so that patients and doctors can make better decisions together that improve long-term kidney health," says James.
More information: Matthew T. James et al. Derivation and External Validation of Prediction Models for Advanced Chronic Kidney Disease Following Acute Kidney Injury, JAMA (2017). DOI: 10.1001/jama.2017.16326
Journal information: Journal of the American Medical Association
Provided by University of Calgary