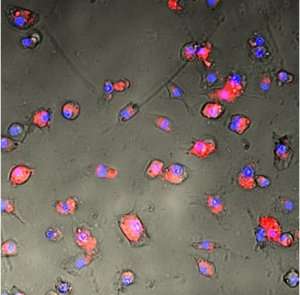
Florescence microscopy image of mouse dendritic cells with mRNA-loaded blood cells.
Even if you don't have allergies yourself, I guarantee you can list at least three people you know who have allergies. Asthma, a respiratory disorder commonly associated with allergies, afflicts over 300 million individuals worldwide.
Seddon Y. Thomas who works at the National Institute of Environmental Health Sciences has been exploring how sensitization to allergens occurs. The work, which she described at a recent session of the Immunology Seminar Series, specifically focuses on the relationship between sensitization and the adaptor molecule MyD88.
MyD88 transfers signals between some of the proteins and receptors that are involved in immune responses to foreign invaders. Since allergies entail inflammation caused by an immune response, Thomas recognized that MyD88 played a role in the immune system's sensitization to inhaled allergens.
Her research aims to discover how MyD88 alters conventional dendritic cells (cDCs) which are innate immune cells that drive allergic inflammation. MyD88 signaling in cDCs sometimes preserves open chromatin—the availability of DNA for rapid replication—which allows gene changes to happen quickly and in turn causes allergic sensitization. Open chromatin regions permit the DNA manipulation that can lead to allergies and asthma.
To conduct her experiments, Thomas examines what happens in mice when she deletes MyD88 from lung epithelial cells and from antigen-presenting cells. Lung epithelial cells form a protective tissue where inhaled air meets the lung and protects from foreign invaders. But sometimes it takes its job a little too seriously and reacts strongly to allergens.
Similarly, antigen-presenting cells are involved in the immune system's mission to protect the body, but can become confused about who the enemy is. When the signaling adaptor MyD88 is removed from lung epithelial cells, the number of eosinophils, inflammatory white blood cells, decreases. When it is removed from antigen-presenting cells, another type of white blood cell, neutrophils, also decreases.
Thomas said this shows that MyD88 is necessary for the inflammation in the lungs that causes asthma and allergies.
In her future research, Thomas wishes to explore dendritic cell gene expression, the molecular pathways controlling gene expression, and how specific types of lung epithelial cells adjust immune responses. Because MyD88 plays a role in the genetic changes, it makes sense to continue research on the genetic side.
Provided by Duke University