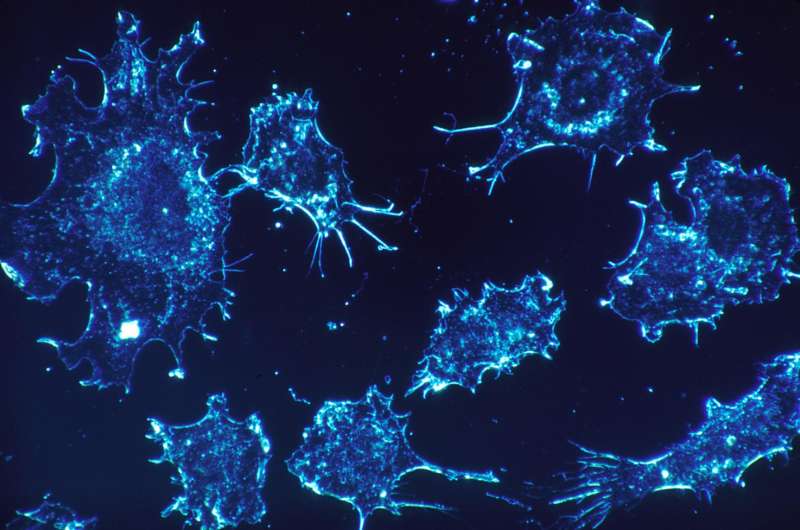
Credit: CC0 Public Domain
A large team of researchers from the U.S., Spain and Australia has found that the efficacy of drugs for treating cancer aimed at targeting particular classes of mutations depends on the type of tumor tissue involved and the nature of the mutations. In their paper published in Nature, the team describes the clinical trial and the results they have seen thus far. Elaine Mardis with the Institute for Genomic Medicine, Nationwide Children's Hospital, in Columbus, Ohio, offers a News & Views piece in the same journal issue outlining the study, and general research of abnormalities in genes linked to cancer and possible new treatment options.
In the past, doctors treated all patients with similar types of cancers in much the same way, but more recent research has shown this is not likely the best approach. This is because not all tumors for specific cancers are alike. As an example, not all lung cancer tumors are the same—their cause and development can vary between patients. For this reason, scientists have been looking for ways to develop customized treatments based on an individual's circumstances. As this new approach has progressed, scientists have found that much of the difference between tumors can be traced back to differences in genes. In this new effort, the researchers have focused on mutations in the ERBB2 and ERBB3 genes because some of them have been found to overexpress HER2 proteins as part of tumor development.
To learn more about the role ERBB2 and ERBB3 play in tumor development, the researchers gave a drug called neratinib to 141 patients with 21 types of cancer (and 42 kinds of mutations) in their clinical trial—it blocks the production of HER2 proteins. They have found that the effectiveness of the drug varied depending on mutational and tissue contexts. Some patients with ERBB2 mutations, they report, responded well to the drug, particularly those with tumors containing alterations in amino acids in extracellular or kinase HER2 domains. Others with tumors expressing HER2 proteins did not respond as well, and those with ERBB3 genes saw no change at all.
The researchers suggest their study has thus far shown that therapies designed to target certain classes of mutations will have to take into account tumor tissue and the nature of the tumors involved.
More information: David M. Hyman et al. HER kinase inhibition in patients with HER2- and HER3-mutant cancers, Nature (2018). DOI: 10.1038/nature25475
Abstract
Somatic mutations of ERBB2 and ERBB3 (which encode HER2 and HER3, respectively) are found in a wide range of cancers. Preclinical modelling suggests that a subset of these mutations lead to constitutive HER2 activation, but most remain biologically uncharacterized. Here we define the biological and therapeutic importance of known oncogenic HER2 and HER3 mutations and variants of unknown biological importance by conducting a multi-histology, genomically selected, 'basket' trial using the pan-HER kinase inhibitor neratinib (SUMMIT; clinicaltrials.gov identifier NCT01953926). Efficacy in HER2-mutant cancers varied as a function of both tumour type and mutant allele to a degree not predicted by preclinical models, with the greatest activity seen in breast, cervical and biliary cancers and with tumours that contain kinase domain missense mutations. This study demonstrates how a molecularly driven clinical trial can be used to refine our biological understanding of both characterized and new genomic alterations with potential broad applicability for advancing the paradigm of genome-driven oncology.
Journal information: Nature
© 2018 Medical Xpress