Search for genetically stable bioengineered gut and liver tissue takes step forward
Before medical science can bioengineer human organs in a lab for therapeutic use, two remaining hurdles are ensuring genetic stability—so the organs are free from the risk of tumor growth—and producing organ tissues of sufficient volume and size for viable transplant into people.
Scientists from the Cincinnati Children's Center for Stem Cell and Organoid Medicine and Yokohama City University (YCU) in Japan report in Stem Cell Reports achieving both goals with a new production method for bioengineered human gut and liver tissues.
The researchers first used a multi-step process of genetic and biochemical manipulation that included the genes FGF, TGF and WNT, which transformed human induced pluripotent stem cells (iPS) into CDX2-positive posterior gut endodermal progenitor cells (PGECs). The protocol is designed to mimic natural embryonic development, and CDX2 is a molecular marker found in gut tissues, according to Takanori Takebe, MD, lead investigator on the study and a physician at Cincinnati Children's and YCU.
Although PGECs are still at an embryonic development stage, they're already programmed to form the gastrointestinal (GI) tract. At this point, however, they aren't specifically queued genetically to form stomach, liver or intestine.
Next, study authors used additional series of progressive genetic and biochemical manipulations, telling PGECs to form human hindgut and liver organoids.
"Compared to gastrointestinal organoids and liver-generated directly from induced pluripotent stem cells, generation from PGECs resulted in robust and genetically stable formation of different tissue GI types, without causing benign tumors called teratomas," said first author Ran-Ran Zhang, PhD, a research fellow at Cincinnati Children's. "Our data also show liver organoids grown from PGECs and transplanted into immunodeficient mice with liver disease grew, functioned well and prevented liver failure."
Study data indicate about 20 percent of mice not receiving liver organoid transplants still survived for 30 days, compared to roughly 60 percent of the mice that received transplants.
Building a Better Organ
Induced pluripotent stem cells (iPS) start out as adult cells, like mature skin cells. They are genetically and biochemically reprogrammed to act like embryonic stem cells. IPS cells have the potential to become any cell type in the human body. This makes them an indispensable research tool for studying human disease and lab-grown human tissues of specific organ systems, such as the GI tract.
But iPS cells and organ tissues grown directly from them are prone to genetic variations and chromosome instability, bringing the possibility of tumor formation. This hurdle to using organ tissues grown directly from iPS cells for applications requires a different approach, said Takebe and his co-authors.
Human organoids have been generated in past studies with progenitor cells, such as the posterior gut endoderm progenitors generated in this study. Research data indicate the progenitor cells are more genetically stable than iPS cells. But previous studies that bioengineered organoids from progenitor cells included the use animal byproducts (reagents and other substances). This makes the resulting organoids unsafe for therapeutic use in people, according to researchers.
In this study, researchers avoid the use of animal byproducts throughout the entire bioengineering process. This includes the initial programming of iPS cells and then their subsequent queuing to become posterior gut endoderm cells.
The Importance of Size
Current bioengineering technologies can safely grow human liver tissues to model and study the progression of specific diseases—such as fatty liver disease—and test for drugs that can treat them. But for lab-generated liver organoids, and other gastrointestinal organoids like intestine, therapeutic viability in patients requires the tissue be highly reproducible and able to grow large enough. They also must function well enough treat or cure medical conditions.
The quantity of PEGC-derived liver organoid tissues in the current study was sufficient for mouse transplant. They also demonstrated the ability to produce highly functional hepatic cells that allowed the mini-livers to filter toxins from the body, the organ's primary role. This is demonstrated in part by the significantly improved survival rate of laboratory mice transplanted with the liver organoids.
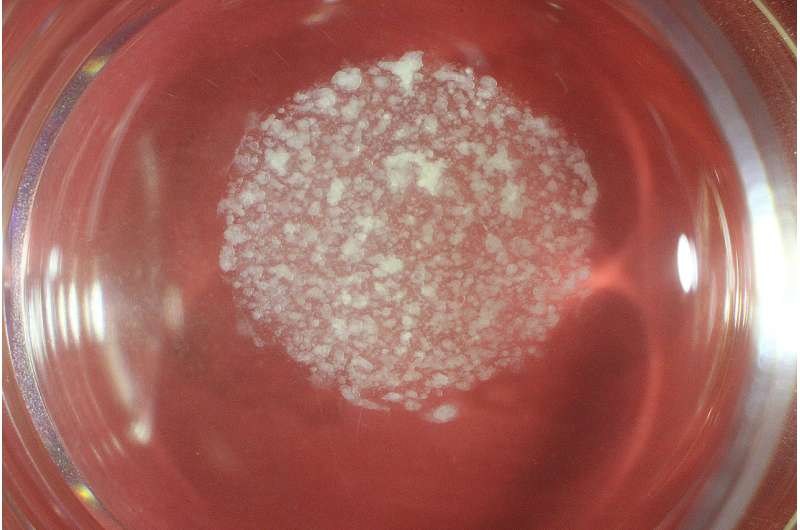
PGEC-derived organoids also demonstrated extensive potential for expansion and elongation. In laboratory cell culture plates, feeder-free PEGCs generated by the researchers multiplied their numbers by 1021 after being re-plated 20 times—-demonstrating their mass production potential.
Following this study, researchers continue refining the bioengineering process, with emphasis on liver organoids. In collaboration with Japan's National Centers for Child Health and Development, the research team is preparing for a clinical trial to transplant a bioengineered liver into a patient, Takebe said.
More information: Stem Cell Reports (2018). DOI: 10.1016/j.stemcr.2018.01.006



















