Team discovers genetic cause of rare high blood pressure syndrome
Twenty-five years ago, an unusual inherited form of high blood pressure was first described in an Australian family. Its genetic cause, however, had remained elusive. Using modern sequencing methods, an international research team led by BIH Johanna Quandt Professor Ute Scholl has succeeded in detecting mutations in a new disease gene (CLCN2)—present in this family and seven others—that are responsible for the development of a familial form of hyperaldosteronism.
More than a billion people worldwide suffer from high blood pressure (hypertension). Prolonged hypertension damages blood vessels, which can result in damage to the heart, kidneys, and brain. Possible consequences include heart attack, kidney failure and stroke. Besides such factors as obesity, salt consumption, and alcohol intake, genetic factors play an important role in the development of hypertension. In some rare cases, familial hypertension is caused by mutations within single genes. These genes play important roles in blood pressure determination, and mutations typically cause early-onset hypertension, even in young children and adolescents. Ute Scholl and a team of scientists from the United States and Australia have now identified a new hypertension disease gene. The study focused on a particular and very rare form of high blood pressure, known as familial hyperaldosteronism type II. This inherited disease causes the adrenal gland to produce too much aldosterone—a hormone that regulates how much salt and water the kidneys retain in the body. Too much of this hormone results in high blood pressure.
Mutation in the CLCN2 gene alters blood pressure regulation
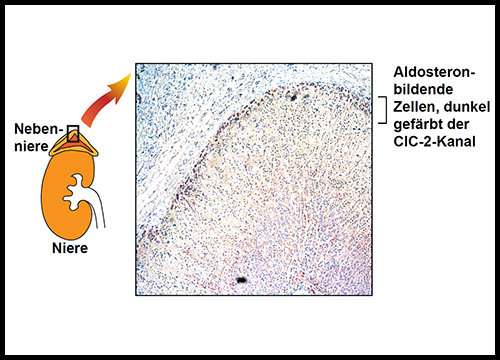
Familial hyperaldosteronism type II was first described in an Australian family 25 years ago. The research team investigated this family along with other patients suffering from hyperaldosteronism in childhood and adolescence. A total of eight families, including the large Australian family, showed mutations in a gene that had not previously been associated with blood pressure regulation. The CLCN2 gene carries information for building a channel in the cell membrane through which chloride ions can pass. In specific cells of the adrenal gland, these chloride channels regulate membrane voltage and aldosterone production. Gene mutations in patients with familial hyperaldosteronism cause changes in the membrane voltage and result in the overproduction of aldosterone, which raises blood pressure.
Study results enable early detection and treatment
Lead author Ute Scholl says, "Patients with suspected familial hyperaldosteronism and their relatives will benefit from our findings because in the future, they can be screened for mutations in the CLCN2 gene."
Study patients also responded to medication that is already used in the treatment of hyperaldosteronism. "For families with familial hyperaldosteronism type II, identifying the genetic cause doesn't just help with early detection of the disease, it also enables targeted treatment," says Scholl. As BIH Johanna Quandt Professor, Ute Scholl and her research group will now use the results from the study to delve deeper into their research at the Berlin Institute of Health. "We plan to further investigate the role of chloride channels in the adrenal gland," says Scholl. "We also try to better understand the regulation of these channels in order to develop improved treatment strategies."
More information: Ute I. Scholl et al, CLCN2 chloride channel mutations in familial hyperaldosteronism type II, Nature Genetics (2018). DOI: 10.1038/s41588-018-0048-5



















