Zika virus could help combat brain cancer
Zika virus, known for causing microcephaly in babies by attacking the cells that give rise to the fetus's cerebral cortex, could be an alternative for treatment of glioblastoma, the most common and aggressive malignant brain tumor in adults. This discovery was made by researchers at the University of Campinas's School of Pharmaceutical Sciences (FCF-UNICAMP) in São Paulo State, Brazil.
"Zika virus, which has become a health threat in the Americas, could be genetically modified to destroy glioblastoma cells," said Rodrigo Ramos Catharino, a professor at FCF-UNICAMP and head of the institution's Innovare Biomarker Laboratory.
Through the mass spectrometry analysis of Zika virus-infected glioblastoma cells, scientists also identified the presence of digoxin, a molecule which induced the death of tumoral cells of skin and breast cancer in previous experiments. The study is described in an article published in bioRxiv, a preprint repository for the biological sciences, and accepted for publication by the Journal of Mass Spectrometry.
Previous research conducted recently in Brazil and elsewhere points to increased mortality rates for human neural progenitor cells (hNPCs) infected by Zika virus, as well as growth inhibition and morphological abnormalities. Alterations in these cells, which are precursors of brain cells and become cortical neurons in embryos and fetuses, may be a cause of microcephaly in babies whose mothers have been infected by Zika. Other studies have shown that the virus is capable of moving into brain cells, modifying the regulation of the cell cycle, and inducing their death.
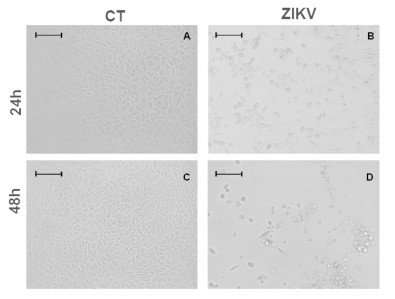
In light of these findings, the researchers at FCF-UNICAMP set out to investigate the effects of Zika virus when it infects glioblastoma cells. To do this, they infected human malignant glioblastoma cells with Zika and recorded microscope images of them 24 hours and 48 hours after infection in order to observe any metabolic alterations (cytopathic effects) caused by inoculation of the virus.
The results of the analysis showed that the glioblastoma cells displayed moderate cytopathic effects 24 hours after infection, such as rounded, swollen cell bodies and formation of syncytia, masses of cytoplasm in which the membrane contains several nuclei. The most severe cytopathic effects were observed 48 hours after infection, with a larger number of rounded, swollen cells, more syncytium formation and pronounced loss of cell integrity, all of which denote cell death.
"The cytopathic effects of Zika infection on glioblastoma cells were observed most clearly after 48 hours. Cell morphology was almost totally altered during this period," Catharino said.
To identify the main compounds (metabolites) produced by glioblastoma cells during infection by Zika, the researchers analyzed the cells using matrix-assisted laser desorption/ionization mass spectrometry imaging (MALDI-MSI). The technique consists of breaking down the atoms or molecules in a sample so that they become charged with more or fewer electrons than the original (ionization) and then separating them by mass/charge ratio in order to identify and quantify them.
The mass spectrometry data were submitted to statistical analysis, which showed that 24 hours after infection, the cells began to produce cardiac glycosides, especially digoxin. Previous in vitro studies conducted by researchers in other countries showed that this molecule was able to reduce the multiplication and increase the mortality of cells from melanoma, the most aggressive type of skin cancer, as well as breast cancer and neuroblastoma, a tumor that typically affects patients aged 15 or younger.
Because digoxin and other cardiac glycosides have been shown to induce cancer cell death, the researchers concluded that infection by Zika triggered synthesis of the molecule in glioblastoma cells and that this phenomenon is probably one of the factors that lead to neuronal cell death. "Digoxin could be the key molecule that activates glioblastoma cell death during Zika infection," Catharino said.
Based on these findings, the researchers suggest that a genetically engineered Zika virus could eliminate the effects of infection and leave only the viral particles that synthesize digoxin. Thus, the virus could be an alternative for the treatment of glioblastoma, which is highly resistant to chemotherapy drugs.
"The use of oncolytic viruses [viruses genetically engineered to destroy tumor cells] is at an advanced stage, especially to treat skin cancer and myeloma [bone marrow cancer]," Catharino said. "Zika could be a candidate for the treatment of glioblastoma."
More information: Estela de O. Lima et al, MALDI imaging detects endogenous digoxin in glioblastoma cells infected by Zika virus-Would it be the oncolytic key?, Journal of Mass Spectrometry (2017). DOI: 10.1002/jms.4058



















