Acute and chronic changes in myelin following mild traumatic brain injury
Preliminary research using mcDESPOT magnetic resonance imaging shows changes in the myelin content of white matter in the brain following mild traumatic brain injury. Myelin changes are apparent at the time of injury and 3 months afterward. For more details, see the article, "Prospective study of myelin water fraction changes after mild traumatic brain injury in collegiate contact sports, by Heather S. Spader, MD, and colleagues, published today in the Journal of Neurosurgery.
According to the Centers for Disease Control and Prevention, an estimated 1.7 million people in the United States sustain a traumatic brain injury (TBI) each year, and about 75% of these TBIs are mild TBIs, which include concussions.
Despite the gentle modifier, "mild" TBIs can cause disabling symptoms (headaches, dizziness, nausea, difficulties with concentration, and others), which in some cases do not resolve for weeks, months, or longer. In some contact-sport athletes, repeated mild TBIs have been linked to chronic traumatic encephalopathy (CTE), a serious neurodegenerative disease that develops later in life and is responsible for severe personality and neurocognitive changes.
What motivated the authors of the present study is the need for better diagnostic and prognostic tools for mild TBI, particularly in people who face greater risks of receiving one or more injuries, such as athletes engaged in contact sports. Thus far, conventional neuroimaging studies have been unable to reveal changes in the brain immediately following concussion and other mild TBIs.
Spader and colleagues tested a specific magnetic resonance imaging (MRI) technique—multicomponent driven equilibrium single pulse observation of T1 and T2 (mcDESPOT for short)—to see if they could find evidence of white matter changes in the brains of male college rugby and football players after mild TBI. White matter tracts (bundles of axons covered by myelin) are susceptible to primary injury from mechanical forces at the time of head injury and again to secondary injury from the swelling and chemical changes that naturally occur in the brain following head trauma.
The researchers assessed white matter changes by measuring the myelin water fraction (MWF)—the ratio of myelin-associated water to total water—in voxels on neuroimaging studies. Changes in the MWF represent changes in the amount of myelin, the white fatty substance that acts as a sheath covering the axons of neurons. The higher the MWF, the more myelin is present. When sufficient amounts of myelin are present and organized, the myelin sheath aids in the swift and accurate transmission of electrical impulses from the nerve cell body across the axon and on to other nerve cells, muscles, or glands. Damage, loss, or disorganization of myelin slows down or impedes this process.
Twenty-three male Brown University students participated in the study: 12 contact sport players (CSPs) who had sustained mild TBIs (one member of the rugby team and 11 football players) and 10 age-matched controls with no such injury (athletes from non-contact sport teams, specifically swimming, fencing, and cross-country).
The CSPs underwent mcDESPOT imaging at the time of diagnosis of mild TBI (within 72 hours after injury) and again 3 months afterward. The controls underwent an identical imaging session. One CSP had also sustained a mild TBI some time before the study commenced; none of the controls had ever sustained a mild TBI.
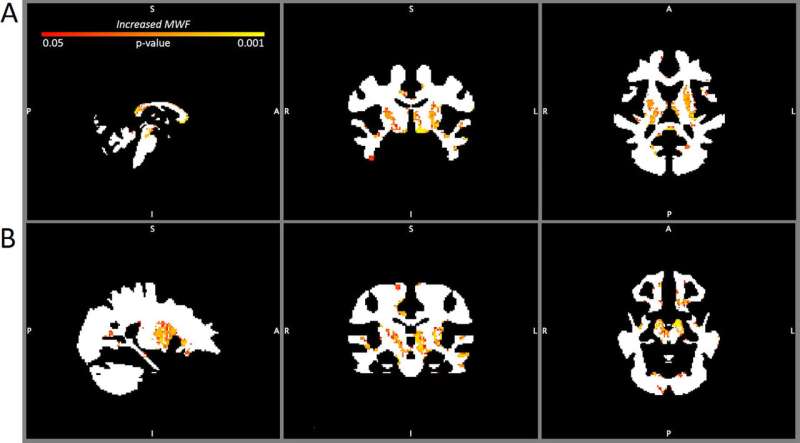
The researchers compared the MWF in the brains of CSPs at each of the two time points with the MWF in the brains of the control players, which served as an uninjured comparison. The researchers also compared the MWF in the brains of CSPs at diagnosis with the MWF measured at the 3-month follow-up examination.
Here are the pertinent findings:
- The MWF in the brains of the CSPs at the time of diagnosis (within 72 hours after injury) was significantly higher than the MWF in the brains of the controls.
- The MWF in the brains of the CSPs 3 months after injury was also significantly higher than the MWF in the brains of the controls.
- The MWF in the brains of the CSPs was higher 3 months after injury than at the time of diagnosis.
These findings are depicted on MWF maps, essentially anatomical masks of white matter over which colored areas show an increased or a decreased MWF.
The increased MWF after mild TBI found in this study demonstrates an active remyelination process after mild TBI. However, as the researchers point out, increased myelin alone is not necessarily a good thing. Animal studies have shown that remyelination following mild TBI may result in disorganized and therefore less functional myelin.
In a related investigation, the researchers compared MWF maps obtained in this study with PET scans obtained in patients suspected of having CTE. The researchers found that the sites of increased MWF in CSPs at both time points corresponded to sites of brain changes in patients suspected of having CTE.
The study is preliminary and no clear clinical ramifications of the MWF changes are apparent. The authors call for further studies in which a true baseline MWF can be determined in CSPs before injury occurs rather than relying on a surrogate baseline MWF from non-contact sport players. The researchers also point out the need for a larger study population. Nevertheless, they note: "this study provides a basis for additional studies aimed at understanding the underlying neuropathophysiology of the brain's recovery from [mild] TBI."
When asked about the study, Dr. Spader replied, "We were surprised by the finding of increased myelin in the contact sports players compared with non-contact sports players at baseline and 3 months after injury. Using the mcDESPOT sequence, we can see that there is a remyelination process after an injury. The next question, however, is to determine if the increased myelin leads to the formation of a type of scar tissue that can cause disorganized signaling in the brain and which can eventually lead to an increased susceptibility to neurodegenerative disorders such as dementia."
More information: Spader HS, Dean DC III, LaFrance WC Jr, Raukar NP, Cosgrove GR, Eyerly-Webb SA, Ellermeier A, Correia S, Deoni SCL, Rogg J: Prospective study of myelin water fraction changes after mild traumatic brain injury in collegiate contact sports. Journal of Neurosurgery published online, ahead of print, May 1, 2018; DOI: 10.3171/2017.12.JNS171597













