Pediatric obesity, depression connected in the brain, study finds
Early-life obesity and depression may be driven by shared abnormalities in brain regions that process rewards, according to researchers at the Stanford University School of Medicine.
Their findings, which will be published online April 23 in Hormones and Behavior, are based on brain MRI scans of children and teenagers ages 9-17 who struggled with depressive symptoms and maintaining a healthy weight. The study is the first to document how concurrent obesity and depression are reflected in the brain in this age group.
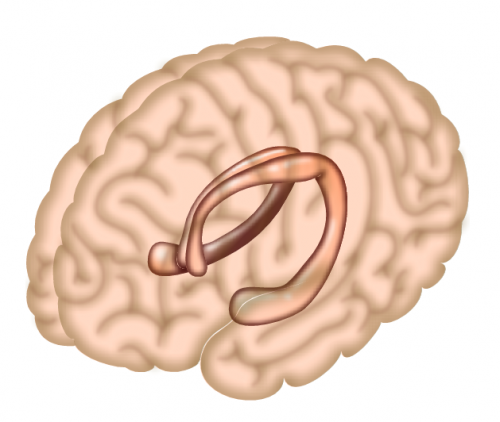
Young people who had both conditions had low volumes in two of the brain's reward-processing areas, the hippocampus and anterior cingulate cortex. The participants' brain abnormalities also were linked to their level of insulin resistance, itself a precursor to diabetes.
"We want to help children and families understand that these conditions are brain-based phenomena," said the study's lead author, Manpreet Singh, MD, assistant professor of psychiatry and behavioral sciences.
Children and teens who have both conditions often feel stigmatized and may hesitate to pursue treatment, said Singh, who is also a child and adolescent psychiatrist at Lucile Packard Children's Hospital Stanford. "We want to destigmatize these issues. Understanding that there's a brain basis may help both children and parents be solution-focused."
Prior Stanford research has shown changes in the same brain networks in adults with obesity and depression. "With this new study, we are trying to understand the earliest age at which this vulnerability begins, and also the earliest time we will be able to intervene when we find the appropriate intervention," said the study's senior author, Natalie Rasgon, MD, PhD, professor of psychiatry and behavioral sciences. "Early intervention is important because, later in life, these are the same brain areas which will ultimately be vulnerable to neurodegenerative processes as well. It's a double whammy."
Cycle of obesity and depression
When obesity and depression begin in childhood, they tend to persist throughout life. Depressed youth may experience a cycle of overeating to try to make themselves feel better, followed by weight gain, ongoing depressed feelings and weight-related bullying that further worsens their depression.
Prior brain-scan research examining obesity or depression individually turned up abnormalities in the brain's reward centers. "Independently, in obesity and depression, the same brain networks popped up, and that was curious to us," Singh said. "We thought maybe that was a link that would help us understand better why these symptoms coexist."
The researchers recruited 42 young participants with a body-mass index greater than the 85th percentile who also had moderate-to-severe untreated depressive symptoms. (All study participants were offered treatment referrals during the study.) Prior to seeking treatment, they were assessed with standard clinical tests and questionnaires to evaluate their level of depression, their experience of pleasure and certain eating behaviors, such as uncontrolled eating and emotional eating. They also had their insulin resistance measured while fasting and after consuming a standard dose of glucose, the sugar in our blood. Insulin helps sugar move from the blood into the body's cells, where it can be used as fuel. When someone becomes insulin-resistant, the hormone works less effectively than usual; insulin resistance is a marker of metabolic dysfunction that precedes Type 2 diabetes. Finally, they had a brain MRI to assess their brain structure and function.
Compared with insulin-sensitive participants, those with more insulin resistance experienced less pleasure from eating, had more eating disinhibition (meaning they were more likely to eat in an unrestrained manner) and also had more generalized anhedonia—that is, difficulty experiencing pleasure.
Better understanding of shared mechanisms
The characteristics of the participants' hippocampus and anterior cingulate cortex were correlated to their levels of insulin resistance and also to their degree of depression, with lower volumes of the two brain regions in children and teens who had more insulin resistance or severe depression, or both.
Greater insulin resistance and greater depression were also linked to stronger connections between the two reward centers. The participants' level of insulin in fasting versus after consuming glucose correlated to the exact location and nature of their brain abnormalities, with somewhat different characteristics in the brains of children whose insulin was higher during fasting rather than after-glucose states.
"We have come closer to understanding the specific shared mechanisms between these syndromes and the commensurate neurofunctional markers that accompany them," the authors write in the study.
Singh's team is now conducting a longitudinal study of a cohort of children and teens, including the participants from this just-completed study, to assess how their brains and clinical symptoms track together over time.
Understanding how the brain differs in young people with obesity and depression also provides scientists with an important baseline for future research to test the efficacy of new treatments, Singh said. In clinical trials of future therapies, brain MRIs may help researchers understand if the treatments have the desired effect. "That's the exciting promise of the next phase of this work: We'll be utilizing the information we get from the brain to develop targeted, mechanistic treatments that we can then track to see if they have the effect they're supposed to have on the brain," Singh said.
The study is an example of Stanford Medicine's focus on precision health, the goal of which is to anticipate and prevent disease in the healthy and precisely diagnose and treat disease in the ill.















