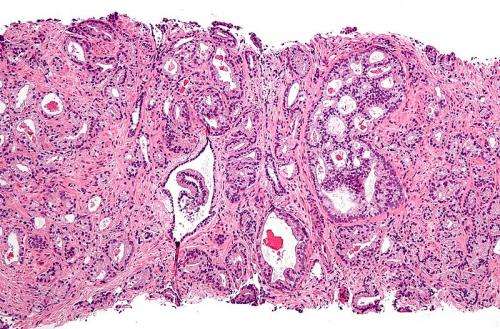
Micrograph showing prostatic acinar adenocarcinoma (the most common form of prostate cancer) Credit: Wikipedia, CC BY-SA 3.0
A software tool to automatically calculate how extensively bones have been infiltrated by prostate cancer is both accurate and speedy, capturing key prognostic information related to survival and the development of symptoms over time.
The software, called the automated bone scan index, was tested in a large, global multicenter study led by Duke Cancer Institute researchers. Findings from the phase 3 study were published May 17 in JAMA Oncology.
"This study describes major improvements over older techniques doctors used to measure bone metastases to predict survival and help guide treatments for patients with advanced prostate cancer," said lead author Andrew Armstrong, M.D., associate professor of medicine and surgery and associate director of the Duke Cancer Institute's Prostate and Urologic Cancer Center.
"It's important to know how widespread metastatic disease is—both for patients to understand the likely course of their disease, and for doctors to determine the best potential treatments," Armstrong said. "It is also a necessary point of reference in clinical trials, to understand whether investigational therapies are working and to quantify and predict possible outcomes."
The current method to measure bone metastases includes a CT or MRI scan along with a nuclear medicine test that involves a manual assessment of the bone metastases. Manual bone scan assessments using a formula based on bone mass and the number of cancer lesions can be done, but that process is both subjective and time-consuming, so is not used regularly in clinic.
The new automated Bone Scan Index, or aBSI, is a software program that scans the radiographic studies and quantifies the degree of bone metastases in a matter of seconds.
In the Duke-led study, 721 men with advanced, recurrent prostate cancer were evaluated using the aBSI software and followed for the duration of their care.
The researchers found that the aBSI technology was significantly better than the older, manual calculation at predicting survival time for the men regardless of how widespread their bone metastases were. Added to other key clinical information, the technology provided prognostic information about patient outcomes and improved the ability to predict the time to symptom progression and the onset of pain.
"It's important for doctors, patients and cancer researchers to have a reliable bone marker to better treat patients and prevent or delay bone metastases," Armstrong said.
Journal information: JAMA Oncology
Provided by Duke University Medical Center