Blockade at the receptor
When chlamydia attacks the human body, the immune system activates. But the bacteria are adapted to defend themselves. Scientists from Würzburg have deciphered new details of their strategy.
Chlamydia trachomatis is a common sexually transmitted disease. More than 131 million people are infected with this bacterium worldwide. If detected at an early stage and treated with antibiotics, the infection can be halted. However, chlamydia often develops without symptoms, and in many cases goes unnoticed. This promotes the spread of the pathogen and increases the chance for secondary infections, e.g. with HIV or Neisseria gonorrhoeae, the causative agent of gonorrhoea.
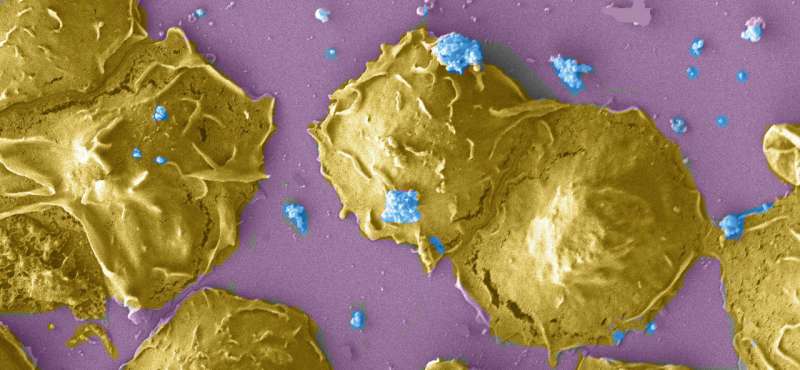
How does Chlamydia trachomatis avoid the attack of the human immune system and thereby also prevent the typical symptoms of an infection? An answer to this question is provided by a new study of scientist of the Julius-Maximilians-Universität Würzburg (JMU). Dr. Karthika Rajeeve and Professor Thomas Rudel, head of the Chair of Microbiology, showed that the bacterium actively deactivates special cells of the immune system, so-called polymorphic nuclear leukocytes (PMNs), and thereby secures its own survival. The results of their work are presented in the current issue of the journal Nature Microbiology.
The struggle between pathogen and immune system follows a defined process in humans: Special leukocytes of the innate immune response become active following an infection. They can take up pathogenic organisms and digest them, and they also secrete special substances that damage bacteria. Leukocytes also form structures called neutrophil extracellular traps that bind microorganisms and kill them. However, many pathogens have developed mechanisms in the course of evolution to destroy these traps, as Chlamydia trachomatis does.
"From previous studies, it was already known that chlamydia is disturbing single steps of the innate immune signal pathways. But the exact mechanism was unknown until now," Thomas Rudel explains. Now, the scientists of the JMU have discovered vital details of these disturbances: "We could prove that free chlamydia even in direct interaction do not activate PMNs. As soon as PMNs attack chlamydia, these cells are paralyzed and do not react to the activation by different stimuli," Rudel says.
The researchers have identified two receptors and a special protein as main players in this battle between bacteria and immune system—the formyl peptide receptor type 1 (FPR1) and type 2 (FPR2) as well as the chlamydial protease like activating factor (CPAF). Both receptors constitute the "antennae" of the immune cells. When they recognize a potential invader, they transmit a signal to the interior of the cell and in this way initiate the immune response. Whereas FPR1 recognizes only particular peptides, FPR2 can bind broader spectrum of proteins, peptides and lipids.
Rudel and his team have now revealed how chlamydia prevent the activation of this process: "We have identified CPAF as the agent which blocks the innate immune response," Rudel says. In their experiments the scientists could show that chlamydia that could not produce CPAF were identified and efficiently killed by immune cells without problem.
Moreover, they identified formyl peptide receptor 2 as a target of CPAF. " FPR2 is cleaved by CPAF and removed from the surface of the immune cells," Rudel says. In contrast, the related FPR1 remains intact in infected cells and mediates its signals. "However, these FPR1-signal pathways seem not to be activated in infected immune cells," Karthika Rajeeve says.
The fact that CPAF plays a crucial role in the process of infection outside of the cell holds the chance for new drugs against the pathogen, according to the scientists. A substance that blocks CPAF could be an appropriate therapeutic agent against chlamydia infections. However, this requires a deeper understanding of the strategies chlamydia employs to paralyze the innate immune system.
More information: Karthika Rajeeve et al, Chlamydia trachomatis paralyses neutrophils to evade the host innate immune response, Nature Microbiology (2018). DOI: 10.1038/s41564-018-0182-y


















