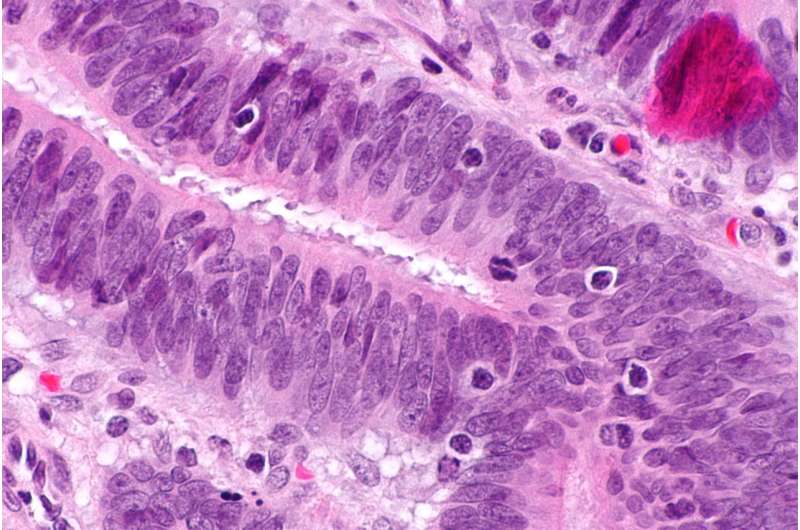
Micrograph showing tumour-infiltrating lymphocytes in colorectal carcinoma. H&E stain. Credit: Nephron/Wikipedia/CC BY-SA 3.0
A team of researchers at Memorial Sloan Kettering Cancer Center has found Lynch syndrome to be associated with more types of cancer than previously thought. The group gave a presentation at this year's American Society of Clinical Oncology meeting outlining their findings.
Lynch syndrome is an inherited condition that results in a higher risk of developing certain types of cancer. Up until now, the elevated risk was thought to be restricted mostly to colon and endometrial cancers. But in this new effort, the researchers found evidence that suggests it can also be associated with other types of cancer, such as prostate, melanoma, ovarian germ cell, sarcoma and mesothelioma—and possibly many others.
Patients who develop endometrial or colon cancer are typically screened for Lynch syndrome, because if markers for it are present, they are likely to be more susceptible to developing it as well. Those who have been identified with it, including the initial patient, can then be offered options to reduce their risk factors or even to treat their tumors—the FDA has an approved therapy list for patients with Lynch syndrome.
The team was conducting a genetic study of tumor samples. They looked at 15,000 samples that included 50 different types of cancer. In particular, they were looking at those with high microsatellite instability (MSI-H) which not only increases the odds of a tumor spreading but of the patient having Lynch syndrome. As part of their analysis, the researchers found that approximately 16 percent of those patients with tumors who had high MSI-H also had Lynch Syndrome. Furthermore, they also found that approximately half of all the tumors they tested that came from patients with Lynch syndrome were not due to colon or endometrial cancers. This, the researchers noted, suggests that many more cancer patients need to be screened for Lynch syndrome than previously.
The researchers conclude that screening for Lynch syndrome accompanying other types of cancers can be done immediately. Doctors need not wait for further results. Patients and their families can start benefiting right away.
More information: Pan-cancer microsatellite instability to predict for presence of Lynch syndrome, abstracts.asco.org/214/AbstView_214_223301.html
Abstract
Background: The success of immunotherapy in microsatellite unstable (MSI-H) and/or DNA mismatch repair deficient (MMR-D) tumors has resulted in routine MSI-H/MMR-D testing in advanced solid tumors. Unlike colorectal (CRC) and endometrial cancer (EC), where this has long been undertaken, the characterization of Lynch syndrome (LS) across heterogeneous MSI-H/MMR-D tumors is unknown. Methods: Through a targeted NGS panel, MSI status was determined via MSIsensor. Scores of < 3, ≥3 to < 10, or ≥10 designated Microsatellite stable (MSS), MSI-Indeterminate (MSI-I) or MSI-H status, respectively. Germline mutations were assessed in MLH1, MSH2, MSH6, PMS2, EPCAM. Immunohistochemical staining (IHC) for MMR-D and tumor signatures in LS patients were assessed. Clinical variables were correlated with MSI and compared via Chi square or T-test. Results: Of 15,045 tumors spanning > 50 cancers , 93.2% were MSS, 4.6% MSI-I, and 2.2% MSI-H. Germline mutations were identified in 0.3% (37/14,020), 1.9% (13/699), and 16.3% (53/326) in the MSS, MSI-I, and MSI-H groups, respectively (p-value < 0.001). 25% of 1,025 MSI-H/MSI-I tumors were CRC/EC, but 50% (33/66) of LS patients had MSI-H/MSI-I tumors less commonly or not previously associated with LS (mesothelioma, sarcoma, adrenocortical, melanoma, ovarian germ cell). LS pts with MSI-H/MSI-I non-CRC/EC tumors only met testing criteria in 63.6% of cases, had lower MSIsensor scores, and were more likely to be MSI-I (MSI-I: non-CRC/EC, 30.3% (10/33) vs CRC/EC 9.1% (3/33); p-value = 0.03). IHC was completed in 86.4% (57/66) of LS MSI-H/MSI-I tumors, with 98.3% MMR-D-concordance. Of LS pts with MSS tumors, 78% had MSH6/PMS2 mutations, but 71% of LS pts with MSI-H/MSI-I tumors had MLH1/MSH2/EPCAM mutations(p-value < 0.001). 89% (33/37) of MSS tumors of LS pts had non-MMR-D signatures. Conclusions: MSI-H/MMR-D is predictive of LS across tumor types and suggests a more heterogeneous spectrum of LS-associated cancers than previously appreciated. Nearly 40% of LS pts with MSI-H/MMR-D non-CRC/EC tumors did not meet clinical criteria for genetic testing, suggesting that MSI-H/MMR-D tumors, regardless of cancer type or family history, should prompt germline testing for the evaluation of LS.
© 2018 Medical Xpress