Food deserts don't benefit from more supermarkets in Chicago, study finds

A new study from researchers at the University of Chicago shows that despite an increase of supermarkets across Chicago, low-income neighborhoods have not reaped the benefits.
The study, published in the July issue of the journal Health & Place, contributes to a growing body of research on food deserts—economically disadvantaged areas where access to healthy food is limited and can affect the health of residents.
The study conducted by researchers at UChicago's Center for Spatial Data Science, along with colleagues at Northwestern University, investigated changes in supermarket access in Chicago between 2007 and 2014, a period spanning the Great Recession.
Marynia Kolak, assistant director for Health Informatics at the Center for Spatial Data Science, and Julia Koschinsky, the Center's executive director, along with their colleagues calculated the average distance to the nearest supermarkets throughout Chicago across census tracts in 2007, 2011 and 2014, and identified areas with low access, high access or changing access over time.
The researchers found that among African-American and socioeconomically disadvantaged residents of Chicago, access to healthy food was persistently poor and worsened in some areas following the economic shocks. However, these findings came even as the total number of supermarkets in Chicago increased over the time range observed.
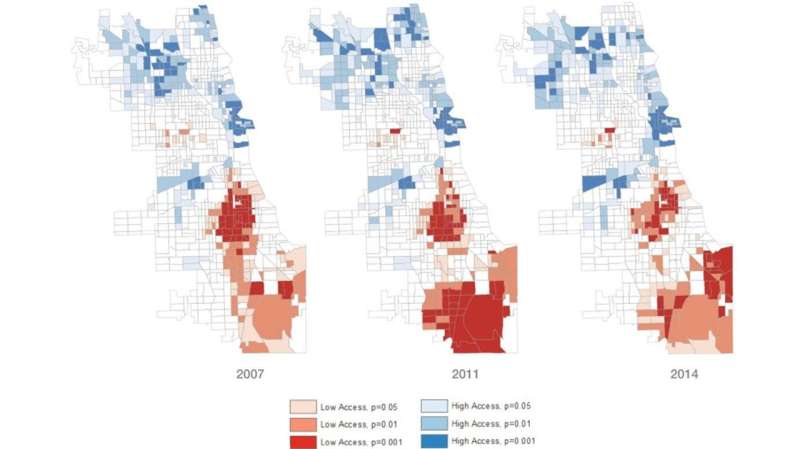
Kolak said closures and re-openings had virtually no impact in areas on the Chicago's North Side neighborhoods she described as a "food oasis." But in South Side neighborhoods, Kolak and her colleagues found that just one store closure jeopardized the food security of an already low-access area.
Kolak said there was a sign of improvement in a swath of neighborhoods, extending southwest of Hyde Park to the Chatham community, where racial segregation existed but with a different socioeconomic makeup than the surrounding area. However, this area shares boundaries with persistent food desert regions, highlighting the complexities of accessibility.
"We really need to get past this binary, 'White equals good food access; black equals bad food access,'" Kolak said. "The real story is much more complicated."
Now that the study is complete, Kolak and researchers plan to continue to better understand issues of food access and work toward better policies with colleagues at the Chicago Department of Public Health.
"I get the sense that the city is really interested in pushing things forward," she said. "But there's a lot more work to be done."
Kolak's interest in the research began in 2013 while she was working at the Institute of Public Health and Medicine at Northwestern mapping the impact of produce carts on communities, which previously had been illegal in Chicago. Spurred by questions of food access and food insecurity, Kolak brought together geography and health researchers to examine the impact of grocery stores openings and closings for their communities.
More information: Marynia Kolak et al. Urban foodscape trends: Disparities in healthy food access in Chicago, 2007–2014, Health & Place (2018). DOI: 10.1016/j.healthplace.2018.06.003















