Visual Abstract. Credit: Nelson et al.
Home visits by trained health representatives in the community can help rural patients become more involved in their own daily diabetes and kidney disease care, according to a study appearing in an upcoming issue of the Clinical Journal of the American Society of Nephrology (CJASN).
For optimal health, patients with chronic kidney disease (CKD) must play an active role in managing their illness. This may be especially true for patients who live in rural communities, where access to care is limited, and in ethnic and racial minorities with a high burden of CKD. As an example, the prevalence of CKD in the Zuni Indians is more than 2.5-fold higher than in the United States general population, and a combination of geography, economic factors, and cultural beliefs has hindered the delivery of healthcare in the Zuni Pueblo, located in rural New Mexico.
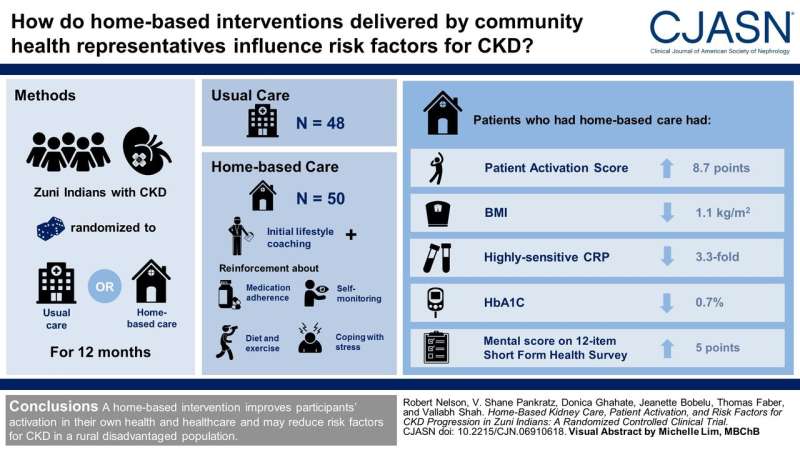
Vallabh (Raj) Shah, Ph.D., FASN (University of New Mexico Health Sciences Center) and his colleagues recently assessed the potential of a pilot kidney care treatment program (funded by the Patient-Centered Outcomes Research Institute) for the management of CKD in Zuni Indians that employed community health representatives under physician supervision to deliver state-of-the-art care in patients' homes. In bi-weekly visits, representatives provided education on health lifestyles, which focused on diet, exercise, alcohol abuse, and smoking, and management of diabetes, hypertension, and high cholesterol.
In the study, 50 individuals received the intervention and 48 received usual care over 12 months. The primary outcome was change in patient activation score, which ranges from 0 to 100 and assesses a participant's knowledge, skill, and confidence in managing their own health and healthcare.
The average patient activation score after 12 months was 8.7 points higher in the intervention group than in the usual care group. Participants in the intervention group had 4.8 times the odds of having a final activation level of at least 3 ("Taking action") than those in the usual care group. The intervention group also showed modest improvements in several clinical measures, including decreases in body mass index, blood glucose levels, and inflammation, and improved mental health quality of life.
"Our study reports that culturally appropriate home-based education from community health representatives can improve patient activation, mental health, and certain CKD risk factors among rural and disparity populations with low health literacy," said Dr. Shah. "Home-based education may be a promising approach for other adults with CKD who experience barriers to accessing health care. Clinics in rural areas could consider offering at-home programs with community health representatives to help patients with kidney disease."
In an accompanying editorial, Joseph Lunyera, MBChB and Clarissa Diamantidis, MD, MHS (Duke University School of Medicine) noted that "several of this study's components highlight pivotal steps for inspiring trust in the medical institution and promoting ownership of CKD care among community members in disadvantaged populations."
In an accompanying Patient Voice editorial, Wendy Rodgers (Milken Institute of Public Health, George Washington University) stressed that the culture of patients is a critical component for quality health care. "Patients need to be heard. They desire to be a part of the solution when it comes to their medical care," she wrote. "This small- sized study had an enormous effect on the health of a vulnerable community by simply adding the seats at the table for the people whose lives will depend on the outcome of the intervention."
More information: Robert G. Nelson et al, Home-Based Kidney Care, Patient Activation, and Risk Factors for CKD Progression in Zuni Indians, Clinical Journal of the American Society of Nephrology (2018). DOI: 10.2215/CJN.06910618
Journal information: Clinical Journal of the American Society of Nephrology
Provided by American Society of Nephrology