Study reveals how brain tumors escape the effects of antiangiogenic drugs
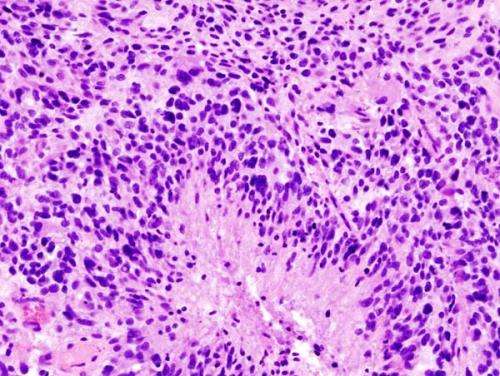
A study led by investigators from Massachusetts General Hospital (MGH) and the University of Cyprus reveals details of a way the dangerous brain tumors called glioblastomas resist the effects of antiangiogenic drugs designed to cut off their blood supply. In their report published in PNAS, the researchers describe how the tumors can spread along existing blood vessels in normal tissue, a process called vessel co-option that can lead to compression of those vessels, reducing the oxygen supply to adjacent tissues and actually stimulating angiogenesis.
"The treatments designed to starve tumors by pruning away blood vessels have provided little or no survival benefits to patients with glioblastoma, says Rakesh K. Jain, Ph.D., director of the Edwin L. Steele Laboratories for Tumor Biology in the MGH Department of Radiation Oncology and senior author of the PNAS report. "Because of its ability to circumvent a tumor's need to develop a new blood supply, vessel co-option can confer resistance to antiangiogenic therapy. Unfortunately this mode of tumor progression is difficult to target because the underlying mechanisms are not fully understood."
To get a better understanding of how cancer cells interact with the vasculature during co-option, Jain and his team followed tumor progression in mouse models of glioblastoma. Using advanced imaging technology they found that treating existing glioblastomas with the antiangiogenic drug cediranib increased the spread of tumor cells along existing blood vessels and away from the primary tumor mass. They also presented evidence that this process causes the compression of co-opted vessels by tumor cells, which can trigger hypoxia-induced angiogenesis.
Using the data from these experiments and from previous studies, the investigators developed a mathematical model that takes into account the biological and physical events driving the process of tumor growth and response to antiangiogenic treatment—from the earliest stages of vascular modification, through vessel co-option to secondary angiogenesis. Designed to integrate events from the cellular and subcellular levels with overall tumor growth, the model's predictions matched the results of several published studies of vessel co-option and further suggested that tumor progression can be more effectively inhibited by combination therapies that block both angiogenesis and co-option.
Jain notes that the possibility that glioblastoma progression can only be stopped by combination therapies has important clinical implications. A previous study from his team identified a specific pathway—the Wnt signaling pathway—as a regulator of vessel co-option in glioblastoma, suggesting that drugs inhibiting that pathway could block co-option. The new model also predicts that targeting co-option before using antiangiogenic drugs would be a better strategy than administering both drugs simultaneously.
"With a number of agents that block Wnt signaling in clinical trials, our work provides the rationale for testing the proposed combination for glioblastoma, a uniformly fatal disease," says Jain, the Cook Professor of Radiation Oncology (Tumor Biology) at Harvard Medical School.
More information: PNAS (2019). DOI: 10.1073/pnas.1818322116


















