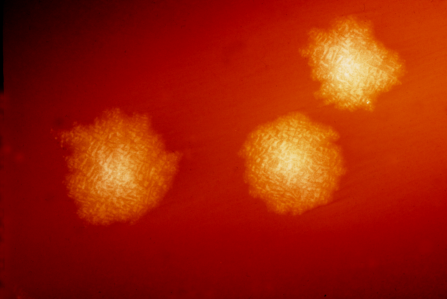
This photograph depicts Clostridium difficile colonies after 48hrs growth on a blood agar plate; Magnified 4.8X. C. difficile, an anaerobic gram-positive rod, is the most frequently identified cause of antibiotic-associated diarrhea (AAD). It accounts for approximately 15–25% of all episodes of AAD. Credit: CDC
Transplanting human donor fecal microbiota into the colon of a patient infected with Clostridiodes difficile (C. diff) may be the best treatment for those not helped by C. diff targeted antibiotics, according to an article in the Journal of the American Osteopathic Association.
C. diff is the most common healthcare-acquired infection in the United States. It affects nearly half a million patients each year and becomes a recurring infection for nearly a third of them. If untreated, C. diff can lead to sepsis and death.
"Twenty five years ago C. diff infections were easier to manage and often resolved with discontinuation of the initiating antibiotic," says Robert Orenstein, DO, an infectious disease specialist at Mayo Clinic and lead author on this article. "However, these infections have become increasingly common and pernicious."
The standard and FDA-approved treatment for C. diff is a course of oral vancomycin, an antibiotic. However, even the medications used to eliminate C. diff can perpetuate the infection by killing off beneficial microbes. Newer antibiotics that more specifically target C. diff have been developed but they can be prohibitively expensive, according to Dr. Orenstein.
"Think of your gut as a forest and C. diff as a weed," says Dr. Orenstein. "In a thriving forest, weeds barely get a foothold. But if you burn the forest down, the weeds are going to flourish."
Unlike antibiotics, which are destructive by definition, fecal transplants or microbial replacement therapies, repopulate the gut with a diverse group of microbes that may block the C. diff's spore from germinating and propagating disease via its toxins. Transplants have several delivery methods, including enemas, capsules and direct instillation, to replace the diverse flora that maintain health and improve metabolism.
Currently, there are no FDA-approved fecal transplant products and performing fecal transplants is considered an investigational procedure. Dr. Orenstein notes there are several companies with products in Phase 3 clinical trials that could come to market as early as 2020. For this reason he strongly urges healthcare providers to refer patients with recurrent C. diff for these trials rather than for fecal transplants. In the meantime, the FDA reserves fecal transplants for patients who have experienced a second recurrence (third episode) of C. diff infection.
C. diff is common in healthcare settings and public spaces and rarely causes problems in people with healthy gut microbiota and immune systems, according to researchers. However, people who are already ill and taking antibiotics, chemotherapy, or proton pump inhibitors—which all greatly disrupt the gut ecosystem—are at risk. Elderly patients are especially vulnerable.
Dr. Orenstein expects the new treatment options will improve outcomes but says physicians need to assume greater responsibility for prevention.
"One of the most effective things physicians can do is become more responsible with antibiotic prescriptions," says Dr. Orenstein. "That means only prescribing when they are clearly indicated, not for colds or viral sinus infections. We also must be especially judicious with elderly patients."
More information: Why Does Clostridium difficile Infection Recur? The Journal of the American Osteopathic Association, May 2019, Vol. 119, 322-326. DOI: 10.7556/jaoa.2019.054 , jaoa.org/article.aspx?articleid=2732400
Provided by American Osteopathic Association