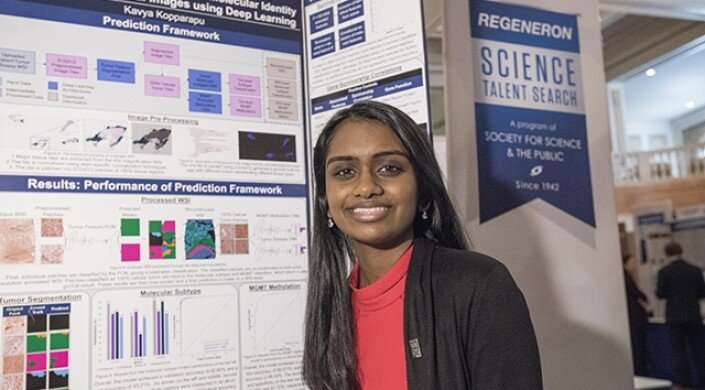
Freshman Kavya Kopparapu created an artificial intelligence platform, called GlioVision, which uses a scanned glioblastoma tumor image to determine the cancer’s molecular and genetic signature in a matter of seconds, with 100 percent accuracy. Credit: Kavya Kopparapu
While reading an article about Sen. John McCain's glioblastoma diagnosis, Kavya Kopparapu was shocked to learn that the prognosis for this aggressive brain cancer has not improved over the past 30 years. With standard treatment, glioblastoma patients typically survive for only about 11 months after diagnosis, according to the American Brain Tumor Association.
"To me, that was really surprising because we know so much more about the brain now, and we have so many improved chemotherapy and surgery techniques," said Kopparapu, who was then a high school junior. "It blew my mind that, despite all of that, we haven't gotten any better at improving patient quality of life and prognosis."
Kopparapu's natural curiosity kicked in, and she started digging into cancer research. While studying the precision medicine pipeline, she noticed a disconnect—while much research has centered on diagnosing and treating cancer, fewer studied focus on using the cancer's genetic signature to find the most effective treatment.
Determining a tumor's molecular cell type through traditional biological methods is slow and costly, which has contributed to this gap in research. The process typically requires a DNA sample and lab tests, and can take weeks or months to complete. Many patients battling this aggressive form of cancer succumb to the disease before their test results are even back from the lab.
Drawing on her background in computer vision and machine learning, Kopparapu decided to see if AI technology could streamline the process.
She used NIH cancer data to build an artificial intelligence platform, called GlioVision, which uses a scanned glioblastoma tumor image to determine the cancer's molecular and genetic signature in a matter of seconds, with 100 percent accuracy.
"Creating the neural network took a lot of trial and error," said Kopparapu, who just wrapped up her freshman year at Harvard. "The entire biopsy image captures a lot of different kinds of tissues, and even in the cancer tissue, there is a high degree of mixing between the healthy cells and the cancer cells."
Kopparapu broke down the super-high-resolution images into smaller pieces to train her algorithms, which zero in on the density and alignment of cells to predict whether specific genes are hyper-expressed or mutated.
"Around 40 percent of glioblastoma patients have a genetic mutation that renders the standard treatment completely ineffective," she said. "So these patients receive all the negative side effects of chemotherapy without any of the benefits of the treatment. That shows why genetic testing is so important."
For Kopparapu, one of the biggest challenges of developing GlioVision was getting up to speed on the latest medical research. She overcame the knowledge barrier by poring over World Health Organization reports on tumor classification and speaking with neuropathologists about the challenges of diagnosis and treatment.
But once she'd refined the neural network so it could make predictions with 100 percent accuracy, she faced challenges from skeptics in the medical field.
"After completing the project, the difficulty and the barrier was figuring out how to explain it to different types of people," she said. "Talking to a computer scientist about the machine learning techniques that I used is very different from explaining to a doctor, from a medical point of view, why the system works."
She's worked to overcome those challenges with the help of peers and mentors in the Harvard Innovation Laboratories, and is relying on their advice as she explores entrepreneurship and potential commercialization of the technology. GlioVision won the Founder Excellence Prize in this year's i3 Innovation Challenge, sponsored by the Technology and Entrepreneurship Center at Harvard.
The platform is currently undergoing clinical trials to test its effectiveness in comparison to traditional methods. If those trials go well, Kopparapu plans to alter GlioVision so it can determine the genetic signatures of different types of cancers.
"For me, the whole point of this research project has been to help someone in the end," she said. "I've spent the past two years meeting so many people—researchers who have devoted their lives to cancer research and patients who have suffered with this aggressive disease. To hear their stories and see how my research could help them has been the most rewarding part of this journey."
Provided by Harvard University