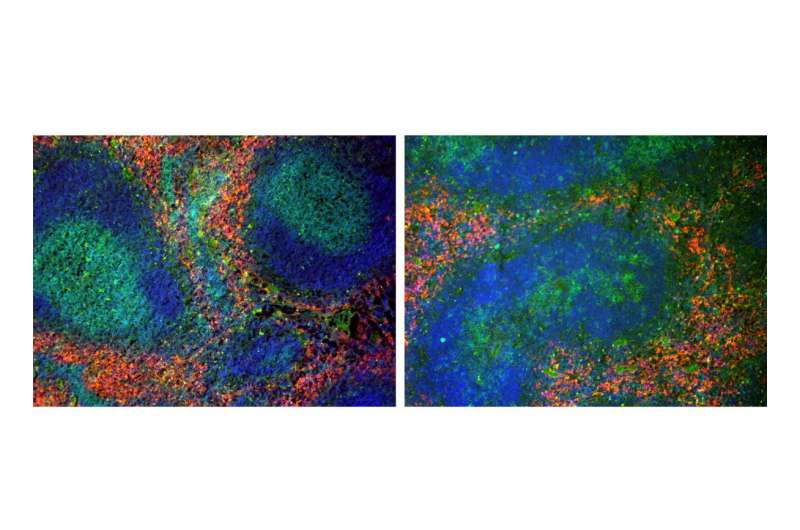
Detection of immune cells using specific antibodies in tissue sections of the spleen of wild type animals (left panel) and mice with T cell-specific deletion of LRH-1 (right panel). (green: T lymphocytes, blue: B lymphozytes, red: macrophages). Credit: Thomas Brunner
The research group around Professor Thomas Brunner at the University of Konstanz discovers the role that the LRH-1 protein plays in the immune system—Inhibiting this protein could help treat inflammatory diseases
Immune cells prevent bacteria, parasites or viruses from entering the body when, for example, the intestinal epithelium is injured. They respond with restricted inflammatory reactions, which are controlled via various processes in the healthy organism. If an organism suffers from Crohn's disease, for example, the immune cells are continuously activated. The research group led by Professor Thomas Brunner at the University of Konstanz has demonstrated that the transcription factor LRH-1 plays a key role in immune cells. That this protein can actually be found in so-called T cells was already confirmed by his team several years ago. The researchers in Konstanz were now able to show that the transcription factor is responsible for ensuring that an organism's immune defense functions properly. If it is not present, no immune response is activated. The researchers view this research result as an opportunity to develop therapeutic approaches or drugs that will control the damaging immune response by inhibiting LRH-1, as in Crohn's disease or liver diseases.
A transcription factor is a protein that ensures that a gene is transcribed and a corresponding gene product is generated. It regulates the so-called gene expression process, which puts the gene's information into effect. The transcription factor LRH-1 is particularly common in the intestine and liver. The elimination of LRH-1 in the epithelial cells of these organs has little effect on them, though. However, the biologists found that the T cells, which are crucial for the immune response, hardly divide when LRH-1 is eliminated. With fatal consequences: T cells have receptors that recognize specific foreign substances. A large number of them are needed to control pathogens such as viruses, which multiply rapidly after infiltrating the body. To fight these viruses, the T cells can usually divide very quickly—even faster than cancer cells—but in a more controlled manner.
"Without the LRH-1 transcription factor, it is practically impossible to trigger immune responses. As a result, the body can no longer protect itself against pathogens," explains Thomas Brunner.
That is the negative aspect. On the positive side, however, this inhibition of the immune cell expansion can be used to treat inflammatory diseases such as Crohn's disease or hepatitis. In the process of continuously fighting either harmless bacteria or viruses, the immune system's permanent response actually damages the organs. The overall aim is to shut down this out-of-control immune response. In fact, a pharmacological inhibitor that can specifically switch off the LRH-1 transcription factor activity already exists. A test has demonstrated that it actually blocks the T cells, thereby reducing the T cell mediated diseases.
Thomas Brunner and his team confirmed that the inhibition of LRH-1 yielded the hoped for results. "In order to test whether or not the inhibitor really works, we administered it to treat experimentally induced hepatitis. It did work. The damage was reduced."
More information: Carina Seitz et al. The orphan nuclear receptor LRH-1/NR5a2 critically regulates T cell functions, Science Advances (2019). DOI: 10.1126/sciadv.aav9732
Juliane Schwaderer et al. Liver receptor homolog-1 (NR5a2) regulates CD95/Fas ligand transcription and associated T-cell effector functions, Cell Death & Disease (2017). DOI: 10.1038/cddis.2017.173
Journal information: Science Advances
Provided by University of Konstanz