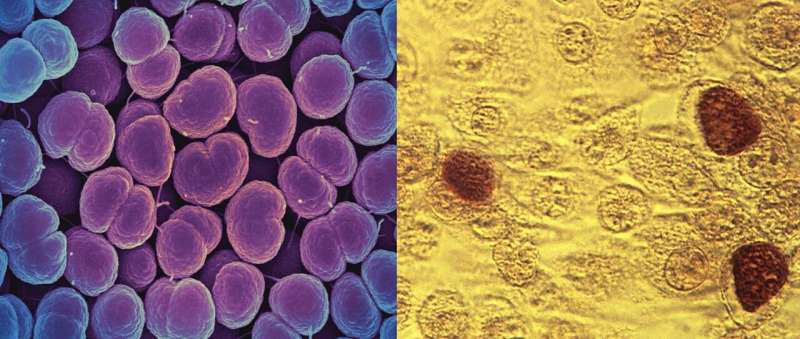
Two sexually transmitted infections, Neisseria gonorrhoeae (left) and Chlamydia trachomatis (right), which can lead to pelvic inflammatory disease (PID). A Johns Hopkins Medicine-led clinical trial shows that a patient-centered, technology-enhanced care program improves PID outcomes in underserved populations. Credit: N. gonorrhoeae image from the National Institute for Allergy and Infectious Diseases and Chlamydia trachomatis image in the public domain via Wikipedia Commons.
A patient-centered, community-engaged program featuring home visits by nurses and mobile phone links to caregivers works better than traditional adult-focused and patient self-managed care systems for treating and managing pelvic inflammatory disease, or PID, among historically underserved teens and young women, a Johns Hopkins Medicine study shows.
In a report on the study appearing in a recent issue of the Journal of the American Medical Association Network Open, Johns Hopkins researchers say that traditional approaches to PID treatment and follow-up care do not address significant age, race and income disparities associated with a population at high risk for recurring sexually transmitted infections (STIs) and subsequent PID.
PID, which can damage female reproductive organs, annually affects an estimated 90,000 women under age 25 in the United States. Left untreated, it can cause scarring of the Fallopian tubes, chronic pelvic pain, ectopic pregnancies, and in severe cases, infertility. According to the Centers for Disease Control and Prevention, 1 in 8 women with a history of PID experience difficulties getting pregnant.
Hoping to reduce PID numbers and impacts, the Johns Hopkins team tested an innovative care program known as technology-enhanced community health nursing (TECH-N) intervention.
"We've known for some time that PID disproportionately affects females between the ages of 13 and 25, and strikes hardest in low-income, minority and urban populations, yet we have continued to treat everyone with the disease in the same manner," says Maria Trent, M.D., M.P.H., professor of pediatrics at the Johns Hopkins University School of Medicine and lead author of the JAMA Network Open paper. "Our study shows that TECH-N gives health care providers a practical, more effective way to team with younger patients to address their specific treatment and follow-up care needs."
To define and measure the impact of a TECH-N program compared with the traditional "standard of care" in treating and managing PID, the researchers conducted a randomized clinical trial of 286 participants, ages 13 to 25, with mild to moderate PID. The patients, primarily from low income and African American populations in Baltimore were recruited over a four-year period from pediatric/adolescent medical clinics and adult emergency departments, associated with the Johns Hopkins University School of Medicine.
Initially, the study participants completed a computer-assisted audio self-interview and were randomly placed into either the standard-of-care or TECH-N intervention groups. All of the patients were tested for two STIs, Neisseria gonorrhoeae and Chlamydia trachomatis; received a full course of antibiotic medication based on federal treatment guidelines; and were given traditional discharge instructions for post-treatment self-care and follow-up visits with health care providers.
Unlike the control group only receiving standard-of-care treatment and follow-up, TECH-N participants also received daily automated text messages on their own cell phones or study-provided, prepaid phones for two weeks after their first treatment session. These messages reminded them to take their medicine and provide caregivers with confirmations that they had done so.
After the 14-day period, the TECH-N group received booster text messages weekly for a month about STI management and prevention.
Additionally, the TECH-N group members received follow-up, in-home visits from a community health nurse at five, 14, 30 and 90 days post-enrollment. During these sessions, nurses examined the patients, collected specimens for STI detection and discussed STI risk reduction tactics, such as proper condom use and partner notification/treatment.
The TECH-N group showed a significant decline in new STIs over the full 90-day study period: 28% compared with 14% for the standard-of-care group. Higher condom use, 21% to 11%, also was seen in those receiving TECH-N intervention.
"These findings show that TECH-N can provide the close, personalized follow-up and support needed after STI diagnosis to successfully treat and manage PID, and subsequently prevent longer-term complications, in a group of urban adolescents and young women currently experiencing a disparity in that care," Trent says.
In spite of economic disparities in the TECH-N study's target population, smartphone technology proved a successful means for reaching them, Trent adds.
"National data demonstrate that 95% percent of sexually active adolescent and young adult women, including those in low-income households, have access to mobile phones with text messaging and internet, and that they are online 'almost constantly,'" Trent says. "In fact, in our study, only 3% of the intervention participants required us to provide them with a cellphone at enrollment."
Based on this first trial's encouraging outcomes, Trent says TECH-N intervention should be seriously considered as an enhancement of current standard-of-care approaches.
"Urban adolescents and young women with PID often struggle to manage the disease on their own, which can escalate to more severe infections and complications such as infertility," Trent says. "Patients also may continue to engage in behaviors that lead to recurring STIs and PID incidence. This study shows the potential for TECH-N-type programs to break that cycle."
More information: Maria Trent et al, Efficacy of a Technology-Enhanced Community Health Nursing Intervention vs Standard of Care for Female Adolescents and Young Adults With Pelvic Inflammatory Disease, JAMA Network Open (2019). DOI: 10.1001/jamanetworkopen.2019.8652
Journal information: JAMA Network Open
Provided by Johns Hopkins University School of Medicine