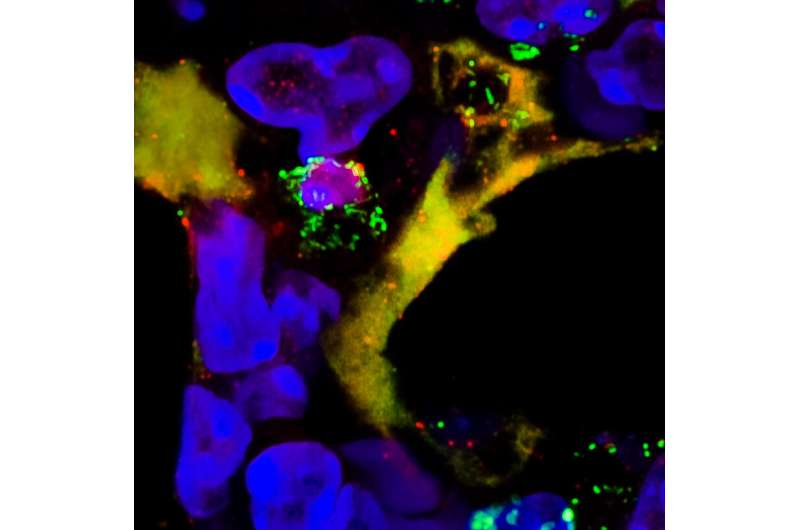
Neutrophil extracellular trap (NET, hippocampa-shaped) in the lung of a mouse exposed to a pro-allergic factor. We also see a neutrophil on his left with the pink nucleus and green granules. Credit: GIGA/University of Liège
In recent decades, asthma has become a major public health problem. The exponential increase in asthma cases in industrialized countries over the past 50 years is due to major changes in the environment. Among these environmental factors: excessive hygiene, ambient air pollution and respiratory viral infections. Until now, the mechanism by which these particular factors induce the development of asthma was unknown.
In a study published in Nature Immunology, Professors Thomas Marichal and Fabrice Bureau and their teams from GIGA ULiège identified a totally unexpected common denominator in different pro-allergic environments: Particular neutrophils are recruited into the lung and are responsible for allergic sensitization and asthma development. This discovery suggests new therapeutic options in the prevention and treatment of allergic asthma.
Coraline Radermecker, the first author of the study, first developed three models of asthma in mice induced by pro-allergic environments: excess hygiene, exposure to ozone (an air pollutant) and infection with the influenza virus. In all three models, only mice exposed to pro-allergic environments and then exposed to mites, major allergens in humans, developed symptoms of allergic asthma. She and her colleagues then observed the recruitment of specific innate immune cells, neutrophils, in the lungs of mice exposed to pro-allergic environments. These neutrophils, once in the lungs, release their DNA, causing inflammation that is conducive to the development of an allergic response such as asthma. Surprisingly, when mice exposed to pro-allergic environments are treated with compounds that prevent the recruitment of these neutrophils or the release of their DNA, the mice are protected from asthma.
A recent study identified this same type of particular neutrophil in the blood of a population of American farmers, the Hutterites, exposed to a very high rate of hygiene and having a very high prevalence of allergic asthma. The latter suggests that these neutrophils are also present in humans and may be involved in the development of asthma in humans.
In addition, a molecule already used in human medicine to treat cystic fibrosis, pulmozyme, could be used to destroy DNA released by neutrophils and prevent the development of asthma in people exposed to high-risk environments.
More information: Locally instructed CXCR4hi neutrophils trigger environment-driven allergic asthma through the release of neutrophil extracellular traps, Nature Immunology (2019). DOI: 10.1038/s41590-019-0496-9 , nature.com/articles/s41590-019-0496-9
Journal information: Nature Immunology
Provided by University de Liege