Study explains why some creams and cosmetics may cause skin rashes
Allergic reactions in the skin can be caused by many different chemical compounds in creams, cosmetics, and other consumer products, but how they trigger the reaction has remained somewhat mysterious.
Now a study suggests the way some chemicals displace natural fats in skin cells may explain how many common ingredients trigger allergic contact dermatitis, and encouragingly, suggests a new way to treat the condition.
The study was led by researchers at Columbia University Irving Medical Center, the Brigham and Women's Hospital, and Monash University and published online today in Science Immunology.
Why some chemicals trigger dermatitis is a mystery
Poison ivy is a commonly known trigger for allergic contact dermatitis, but the reaction can also be caused by many ingredients of consumer products and has become highly prevalent in industrialized nations.
The reaction begins if the immune system's T cells recognize a chemical as foreign. Research suggests that generally small chemicals must bind to a larger protein in order to become visible to T cells, and few chemicals do this by undergoing a chemical reaction inside our body.
"However, many small compounds that trigger allergic contact dermatitis lack the chemical groups needed for this reaction to occur," says study co-leader Annemieke de Jong, Ph.D., assistant professor of dermatology at Columbia University Vagelos College of Physicians and Surgeons.
"These small chemicals should be invisible to T cells, but they're not."
Subhed: Skin cells unmask allergy-inducing chemicals
De Jong and her colleagues suspected that CD1a, an abundant molecule on the skin's Langerhans cells (immune cells in the skin's outer layer) might be responsible for making these chemicals visible to T cells.
In the current study, conducted with human cells in tissue culture, the researchers found that several common chemicals known to trigger allergic contact dermatitis were able to bind to CD1a molecules on the surface of Langerhans cells and activate T cells.
These chemicals included Balsam of Peru and farnesol, which are found in many personal care products, such as skin creams, toothpaste, and fragrances. Overall, the researchers identified more than a dozen small chemicals that activated T cells through CD1a.
"Our work shows how these chemicals can activate T cells, but since we did not do a patient study, we have to be cautious about claiming that this is definitively how it works in allergic patients," de Jong says. "The study does pave the way for follow up studies to confirm the mechanism in allergic patients and design inhibitors of the response."
New Ideas for Treatment
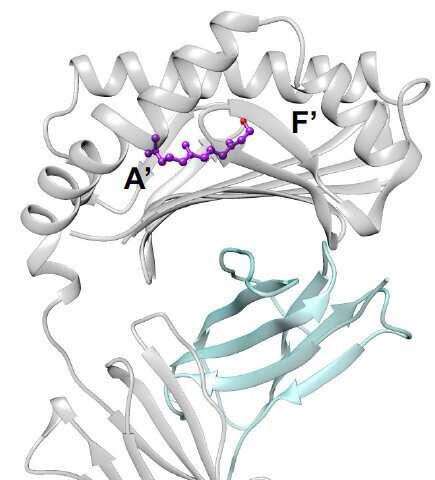
CD1a molecules normally bind the skin's own naturally occurring fats in its tunnel-like interior. These fats protrude from the tunnel, creating a physical barrier that prevents CD1a from interacting with T cells.
Based on structural work done at Monash University, farnesol, one of the allergens identified in this study, was shown to hide inside the tunnel of CD1a, displacing the resident natural fats. "This displacement makes the CD1a surface visible to the T cells resulting in an immune reaction" de Jong says.
This discovery raises the possibility that allergic contact dermatitis could be stopped by applying competing fats to the skin to displace ones triggering the immune reaction. "From previous studies, we know the identity of several fats that can bind to CD1a but won't activate T cells," she says.
Currently, the only way to stop allergic contact dermatitis is to identify and avoid contact with the offending chemical. Topical ointments can help sooth the rashes, which usually clear up in less than a month. But in severe cases, physicians may prescribe oral corticosteroids, which are broadly anti-inflammatory and immune suppressive, but can leave patients vulnerable to infections and other side effects.
More information: S. Nicolai el al., "Human T cell response to CD1a and contact dermatitis allergens in botanical extracts and commercial skin care products," Science Immunology (2019). immunology.sciencemag.org/look … 6/sciimmunol.aax5430


















