Credit: Institute of Cancer Research
More targeted forms of radiotherapy can effectively treat bladder cancer which has spread to the lymph nodes of the pelvis, according to a new clinical trial.
This form of cancer—known as node positive bladder cancer—has a particularly poor prognosis and hasn't usually been treated with radiotherapy. Patients are traditionally offered palliative treatment to manage their pain and other symptoms instead.
Scientists at The Institute of Cancer Research, London, in conjunction with researchers and clinicians at The Royal Marsden NHS Foundation Trust, conducted a phase II clinical trial assessing the use of radiotherapy in patients with bladder cancer which had spread to the pelvic lymph nodes.
Patients whose cancer had not yet spread to the pelvic lymph nodes, but who were considered to have cancer at a high risk of spreading to the nodes, were also included in the study.
Intensity-modulated radiotherapy
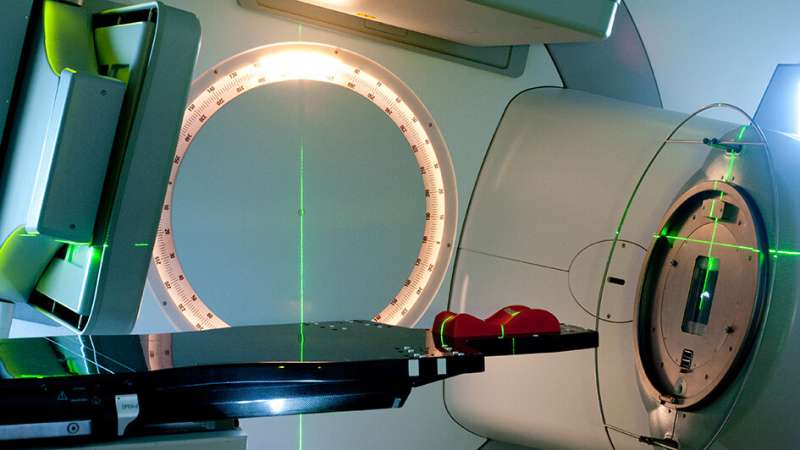
The work sought to assess the use of a type of radiotherapy called intensity-modulated radiotherapy (IMRT) to treat the bladder and pelvic lymph nodes and observe any toxic effects that resulted from the treatment.
IMRT is a type of radiotherapy in which the shape of the radiation beam is guided to fit closely around the shape of the tumour, while the machine moves around the patient's body.
Some patients who have chemotherapy and surgery to remove their bladder and pelvic lymph nodes do achieve control of their disease, but radiotherapy is not typically offered as part of the treatment plan.
Concerns around the use of radiotherapy in bladder cancers centre on the risks involved in the toxicity caused by treatment of the whole pelvic area with radiotherapy, which can cause symptoms such as diarrhoea, incontinence and rectal bleeding as the functions of the healthy tissues surrounding the cancer are disrupted by the radiation.
The severity of these symptoms is rated on a scale in grades from Grade 0 to Grade 4.
Maximising radiation delivered to tumours
Professor Robert Huddart, Professor of Urological Cancer at the ICR and Consultant in Urological Oncology at The Royal Marsden, who led the study, said:
"We hypothesised that using IMRT would give the best chance of maximising the dose of radiation which is delivered to the tumours, while minimising the dose of radiation delivered to healthy cells, reducing the risk of toxic side effects in patients."
The study was published in the journal Clinical Oncology and was conducted with part-funding from National Institute for Health Research's Biomedical Research Centre at the Royal Marsden NHS Foundation Trust and the Institute of Cancer Research.
Some of the patients in the study had already received chemotherapy to try to shrink the tumour before beginning radiotherapy treatment, known as neoadjuvant chemotherapy. This allowed the researchers to assess whether chemotherapy alone, or chemotherapy in conjunction with radiotherapy provides the best chances for these patients.
37 patients received IMRT in this study. Radiotherapy treatment was targeted at four separate areas—the whole bladder, pelvic lymph nodes, tumour bed and involved lymph nodes. CT scans were used to look at these four areas and plan the radiotherapy treatment for each patient.
Radiotherapy was delivered daily to patients using IMRT supported by cone-beam computed tomography imaging—a type of CT scan which allows clinicians to produce a virtual 3-D image of the area to be treated.
After completion of the course of radiotherapy, patients were reviewed at four, eight and 12 weeks to check for any toxic effects from treatment. Patients were then followed up every six months up to three years, and then annually up to five years.
Although most patients—between 70.3 percent and 82.4 percent—suffered negative side effects, including diarrhoea and increased urinary frequency, most of these were mild to moderate and short-lived resolving in the weeks following treatment.
By one year after treatment, the levels of side effects had reduced dramatically. Just 5 percent of patients were experiencing side effects at the more severe end of the scale—Grades 3 and 4—one year after treatment. A check at four years reported that none of the patients was experiencing side effects at the more severe end of the scale.
'IMRT radiotherapy is a promising new option'
The five-year overall survival rate was 34 percent, which is comparable to the survival rate of node-positive bladder cancer patients who receive chemotherapy and surgery alone.
Professor Robert Huddart added: "This trial shows that delivering IMRT to the pelvic lymph nodes and bladder is feasible as a part of a treatment plan for patients with node positive bladder cancer, and patients are able to receive and tolerate appropriate doses of radiation.
"More work needs to be done to combine radiotherapy and chemotherapy to increase the chances of survival and decrease the chances of relapse but these results show that IMRT radiotherapy is a promising new option for this group of patients."
Provided by Institute of Cancer Research