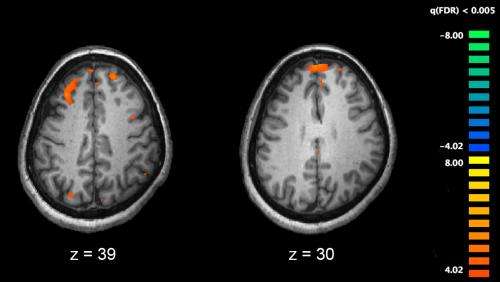
Functional magnetic resonance imaging (fMRI) and other brain imaging technologies allow for the study of differences in brain activity in people diagnosed with schizophrenia. The image shows two levels of the brain, with areas that were more active in healthy controls than in schizophrenia patients shown in orange, during an fMRI study of working memory. Credit: Kim J, Matthews NL, Park S./PLoS One.
A better understanding of the lived experience of people with schizophrenia would enable clinicians to help patients live with their condition, alongside treating symptoms with medication and psychotherapy, say experts at the University of Birmingham.
According to researchers at the University, this approach would involve developing an understanding of 'self-disturbance' in schizophrenia—in which patients' sense of connection to themselves and to their actions is disrupted.
In a new paper, published in The Lancet Psychiatry, researchers assessed existing theories around how this sense of self is constructed by schizophrenia patients. These theories explore the ways in which patients might feel their thoughts do not belong to them, or the irregularities in the way people with schizophrenia might perceive the world.
Rather than attempting to find out which theory is right, the authors argue these different approaches should be drawn together to inform clinical practice.
The authors also argue for the integration of more recent computational 'prediction error' models which attempt to explain delusion and hallucination in terms of a mismatch between expectation and experience.
Dr. Clara Humpston, co-lead author of the study, explains: "Clinical intervention frequently focuses on correcting the patient's thoughts and perceptions. We think this effort is misplaced. Instead, well-informed clinicians might focus on how patients can lead a fulfilling life with their symptoms."
"Key to this is acknowledging that what we consider to be 'real' is likely to be different for the clinician and the patient. This conflict is likely to be particularly pronounced in the early stages of the illness where patients are likely to show a lack of insight into their behaviour or the condition itself. However, 'reality' is still constructed by similar neural and experiential mechanisms for both clinician and patient. Clinicians must not forget how they approach the discrepancies in reality can make a lasting impact on the patients' willingness to engage as it's often in the early stages of an illness that intervention can be most successful."
Dr. Humpston added: "This sort of approach requires clinicians to listen more carefully with an open mind, putting aside what they would interpret as 'real'. With this understanding, clinicians are better able to engage with the patient, share clinical knowledge and come to a mutually understood plan for care and recovery."
Professor Matthew Broome, co-lead author, said: "Despite decades of working in parallel, we're at an important time in mental health research and practice where new approaches in computational neuroscience are engaging meaningfully with detailed accounts of personal experience and phenomenology, allowing science to address the issues that matter most to those who may experience psychosis and schizophrenia."
More information: Thinking, believing and hallucinating self in schizophrenia, The Lancet Psychiatry (2020). www.thelancet.com/journals/lan … (20)30007-9/fulltext
Journal information: The Lancet Psychiatry
Provided by University of Birmingham