Real-world evidence empowers personalized decisions about weight-loss surgery
With today's JAMA Surgery publication of findings on how many adults see their Type 2 diabetes go away and come back following weight-loss surgery, the PCORnet Bariatric Study now provides patients and their doctors with a more complete picture about the comparative benefits and risks of the two most commonly used bariatric procedures.
The study's findings on diabetes as well as earlier findings on weight loss and health risks are now being incorporated into a decision aid to empower patients consulting with their clinicians to make personalized decisions about weight-loss surgery.
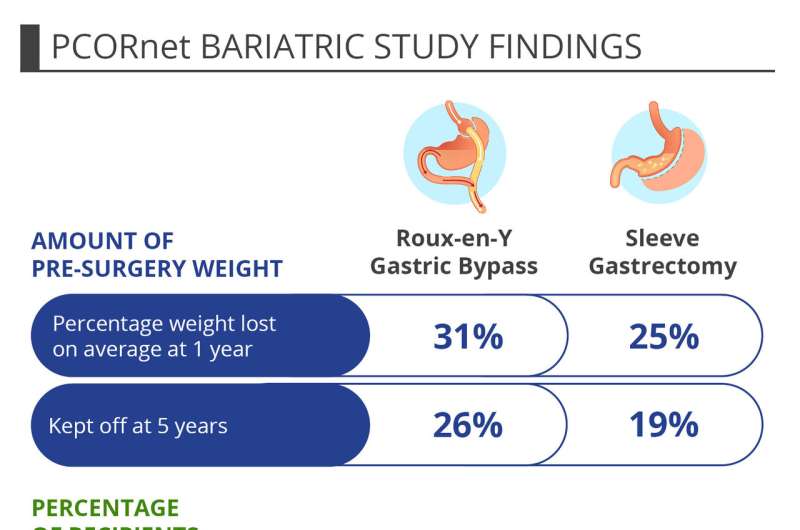
People with severe obesity contemplating weight-loss surgery face a choice between the longer-used Roux-en-Y gastric bypass procedure or a newer and somewhat simpler surgical approach, sleeve gastrectomy, which now accounts for two out of every three bariatric surgeries performed in the United States.
Funded by the Patient-Centered Outcomes Research Institute (PCORI), the PCORnet Bariatric Study is the largest to date to compare these procedures. Its prior findings on weight loss and maintenance among adult patients and rates of short-term health risks were reported in Annals of Internal Medicine. Findings on rates of long-term problems requiring reoperations and other interventions appeared in JAMA Surgery.
"Taken together, the evidence from the PCORnet Bariatric Study is vital to enabling patients and their health care providers to weigh the tradeoffs of the procedures and make personalized decisions based on what matters most to each patient," said PCORI Interim Executive Director Josephine P. Briggs, M.D. "This study is exemplary of how the comparative effectiveness research that PCORI funds can empower better-informed health care decision making."
The findings are important because obesity in U.S. adults hit a 20-year high in 2017-2018, according to new data from the Centers for Disease Control and Prevention, with 42 percent of U.S. adults considered obese and about 9% of adults classified as severely obese. In addition, sleeve gastrectomy has quickly become the most commonly performed bariatric procedure in the United States, but because it was introduced in the country less than a decade ago, less evidence has been available to compare it to bypass.
"More people with severe obesity should be having conversations about the role of bariatric surgery, which has been underused because of concerns about safety and weight regain," said the study's lead co-principal investigator David Arterburn, M.D., M.P.H., an internist and senior investigator at Kaiser Permanente Washington Health Research Institute in Seattle. "The results of the PCORnet Bariatric Study show that the overwhelming majority of patients maintain successful weight loss long term, especially after bypass. But bypass patients had a higher risk of subsequent operation and hospitalization."
"As with many health care options, no one weight-loss surgical procedure is the best choice for every patient because tradeoffs are associated with each," added co-principal investigator Kathleen McTigue, M.D., M.P.H., M.S., an associate professor of medicine and epidemiology at the University of Pittsburgh. "The choice requires personalized decision making that involves weighing the evidence about the pros and cons along with each person's individual circumstances and preferences."
For example, one person might decide it's most important to lose and keep off as much weight as possible and may be willing to accept the greater risks that come with gastric bypass. Meanwhile, a second person with very similar medical history may decide it's most important to minimize the chances of additional operations and hospitalizations that require time away from work and accept the lesser weight loss associated with sleeve gastrectomy.
To make the findings more accessible to patients and health care providers to use in decision making conversations, the research team is incorporating the findings into a decision aid as part of a PCORI-funded implementation project. This tool is part of a broader process for shared decision making between doctors and patients that the team is designing at two health systems, working with four bariatric clinics, nine surgeons and dozens of primary care providers.
The PCORnet Bariatric Study was able to provide findings from the largest sample sizes available to date through its use of tens of thousands of medical records, accessed via PCORnet, the National Patient-Centered Clinical Research Network.
Developed with funding from PCORI, PCORnet harnesses the power of real-world data drawn from electronic health records, claims data and other sources to generate real-world evidence. The network enables researchers to access aggregated, de-identified data to conduct research on large sample sizes.
Both PCORnet and PCORI emphasize patient guidance and partnership in studies. People who have had weight-loss surgery served as co-investigators and helped to refine the study question, select outcomes to study, interpret the findings and present the results.
More information: JAMA Surgery (2020). DOI: 10.1001/jamasurg.2020.0087 , jamanetwork.com/journals/jamas … 1/jamasurg.2020.0087


















