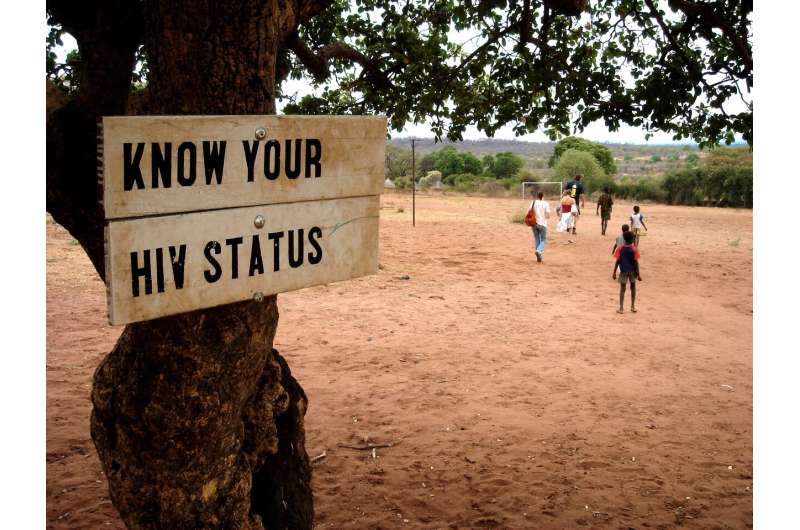
Know your HIV status. Credit: Jon Rawlinson (CC BY 2.0) https://www.flickr.com/photos/london/75148497/in/photostream/ https://www.flickr.com/photos/london/ https://creativecommons.org/licenses/by/2.0/
As global COVID-19 cases multiply, medical researchers fear for how the pandemic will impact the world's most marginalised populations. In particular, people living with HIV in resource-poor, low-income countries are a critical concern, as they may be at risk of more severe outcomes from viral infections.
The Kirby Institute at UNSW Sydney will coordinate a multi-country study to determine risk factors for COVID-19 among people living with HIV, and to collect crucial information to inform strategies for clinical care in low-income countries.
The research is funded by Unitaid: Supporting innovation for global health, and ViiV Healthcare and will be conducted across up to 15 countries, through partnership with Ezintsha Wits RHI (Johannesburg, South Africa), the University of Montpellier, the French Agency for Research on AIDS and Viral Hepatitis (ANRS), the Central Hospital of Yaoundé, Cameroon, Geneva University Hospitals, and the University of Liverpool.
Globally, there are 37.9 million people living with HIV, and most people with HIV live in low-income countries, where health systems were stretched well before COVID-19.
"There is an urgent and critical need to establish how COVID-19 affects people living with HIV in low-income settings, so that we can plan for the health needs of these populations" said the Kirby Institute's Associate Professor Mark Polizzotto, who is leading the study.
"High-income countries are struggling, and in many cases failing, to contain their COVID-19 epidemics. Where they have had success, it has been down to sophisticated public health systems, and co-ordinated, well-resourced strategies to control the movement of people," continued Associate Professor Polizzotto. "But in low-income settings, this simply won't be possible. People live in crowded accommodations, and without government safety nets, and it is next to impossible to stop people from going to work. Add to this the high numbers of people living with HIV, and you can understand why there's global concern about the potential impact of COVID-19 in Africa and other resource-poor settings in our region."
The research collaboration, the first of its kind globally, is called COHIVE, and it will bring together four existing HIV treatment trials and follow the participants on these trials who also test positive for COVID-19.
"The existing clinical trials being coordinated by this group of researchers encompass a range of HIV therapies, HIV populations, and geographic regions—including particularly vulnerable populations like pregnant women living with HIV—ensuring that we capture the full spectrum of this global public health emergency as it to relates to people living with HIV," said Dr. Philippe Duneton, Unitaid's Executive Director.
"This is why we have dedicated further funds to add the COVID-19 observational component to these trials. It's exactly these kinds of collaborative innovations that Unitaid has supported for many years, and this project is one of the many ways we've quickly adapted to redeploy our resources to help those most vulnerable to COVID-19."
Associate Professor Polizzotto said that the COVID-19 public health crisis requires extensive collaboration, a sharing of knowledge and most importantly an awareness of our shared humanity. "When the most disadvantaged in society have the same tools to protect themselves from COVID-19 as the wealthy, we'll know we've done everything we can," he said.
Provided by Unitaid ViiV Healthcare