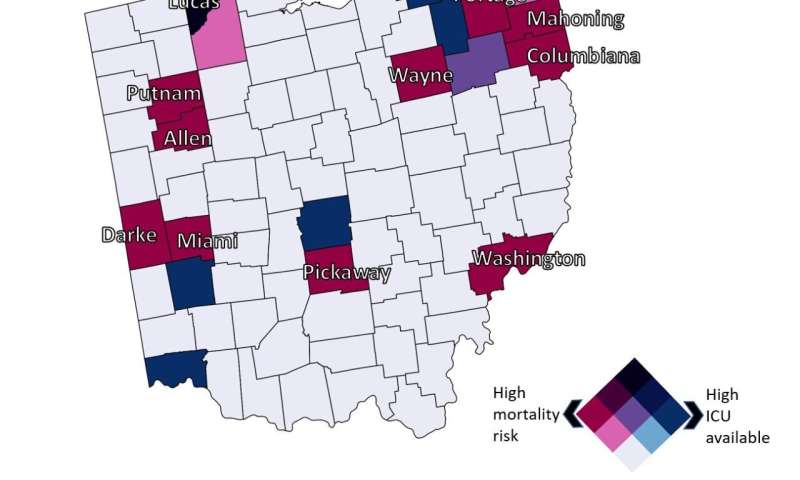
UC identified counties where mortality risk (red) and ICU availability (blue) are highest. Credit: Geospatial Health Advising Group
Residents in eight states have a higher risk of dying from coronavirus compared to the rest of the country, according to a new geospatial analysis by the University of Cincinnati. Likewise, those living in some rural counties in Ohio also face higher risks than other Ohioans based on infection rates and the availability of critical-care resources.
The Geospatial Health Advising Group submitted a new public health policy brief this week to the Ohio Department of Health. Researchers found that the virus is having a disparate impact across the United States. Some people face a much higher risk of dying from the virus than others based simply on where they live.
Nationally, residents in eight states face a higher than average risk of dying from COVID-19: Indiana, Michigan, Colorado, Connecticut, Massachusetts, Louisiana, New Jersey and Washington.
"Overall, we found that COVID-19 related risk is not the same everywhere," said Diego Cuadros, assistant professor of geography in UC's College of Arts and Sciences. He is director of UC's Health Geography and Disease Modeling Laboratory.
"Most counties with high COVID-19-related mortality risk had middle-to-low critical-care capacity," he said.
County-level analysis
UC used county-level data from Johns Hopkins University through May 5 to examine the national mortality risk by state and county, said Neil MacKinnon, dean of the UC James L. Winkle College of Pharmacy.
UC researchers considered the age of the population and the capacity of intensive care unit beds, among environmental and sociodemographic factors.
"That's the power of a multivariate analysis," MacKinnon said. "Just because a state has more seniors doesn't mean you'll see more cases."
UC identified about a dozen mostly rural counties across Ohio in which the risk of dying from COVID-19 was twice as high compared to the state average: Allen, Columbiana, Darke, Lucas, Mahoning, Miami, Pickaway, Portage, Putnam, Washington and Wayne.
What explains the higher risk? The report suggests that socioeconomic and environmental factors could exacerbate mortality risk in this population. These counties also could be vulnerable because of comparatively limited health care capacity.
UC's report suggests boosting the pandemic response in these counties.
"We anticipate that the results from this study can be used to guide the development of strategies for identification and targeting prevention efforts in these vulnerable high-risk counties," Cuadros said.
Ohio Gov. Mike DeWine addressed the disparity in health outcomes on Thursday in a news conference.
"Disparities in health and health care are intertwined with social and economic conditions, as well as race, ethnic background, age and even geography," DeWine said. "Knowing that some of our citizens are disproportionately at risk based simply upon their ZIP code is something that should shock all of us. We have an obligation to be even more mindful in our response to helping those at higher risk."
UC's Geospatial Health Advising Group on April 30 released a public health policy brief on COVID-19 projections in Ohio under different social distancing scenarios as the state seeks to reopen. The group is composed of researchers from the departments of geography and mathematics in UC's College of Arts and Sciences, the UC College of Pharmacy and Cincinnati Children's Hospital Medical Center.
Provided by University of Cincinnati