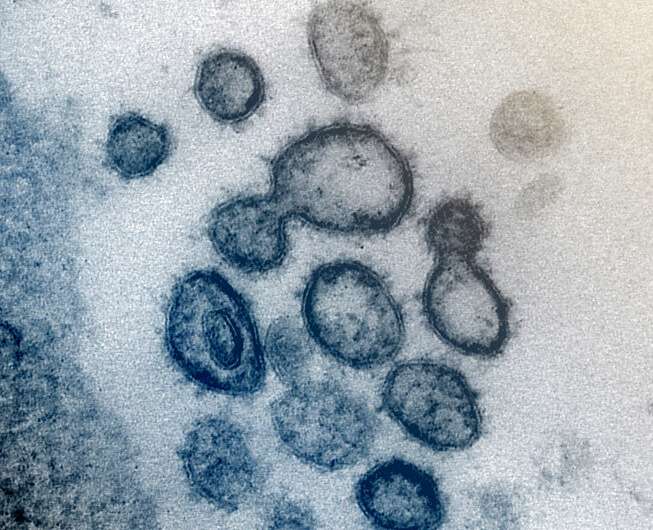
This transmission electron microscope image shows SARS-CoV-2 -- also known as 2019-nCoV, the virus that causes COVID-19 -- isolated from a patient in the US. Virus particles are shown emerging from the surface of cells cultured in the lab. The spikes on the outer edge of the virus particles give coronaviruses their name, crown-like. Credit: NIAID-RML
A new study led by Marshall University researcher M. Jeremiah Matson found that environmental conditions affect the stability of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in human nasal mucus and sputum.
Matson, the lead author on a study published earlier this month as an early release in Emerging Infectious Diseases, the journal of the Centers for Disease Control and Prevention (CDC), is a student in the combined Doctor of Medicine and Doctor of Philosophy in Biomedical Research program at the Marshall University Joan C. Edwards School of Medicine.
SARS-CoV-2, the virus that causes the disease known as COVID-19, was found to be less stable at higher humidity and warmer temperatures. In the study, SARS-CoV-2 was mixed with human nasal mucus and sputum specimens, which were then exposed to three different sets of temperature and humidity for up to seven days. Samples were collected throughout the study and analyzed for the presence of infectious virus as well as viral RNA alone, which is not infectious. Viral RNA was consistently detectable throughout the seven-day study, while infectious virus was detectable for up to approximately 12-48 hours, depending on the environmental conditions.
"The COVID-19 pandemic has been a sobering reminder that infectious diseases continue to be a major public health threat and require sustained research commitment," Matson said. "While this is a small study that only addresses the potential for fomite [an object that may be contaminated with infectious agents] transmission, which is thought to be less important than droplet transmission for SARS-CoV-2, it nevertheless is informative for public health risk assessment."
In a second study, also released this month in Emerging Infectious Diseases, Matson was part of a team of researchers that evaluated the effectiveness of N95 respirator decontamination and reuse against SARS-CoV-2. Vaporized hydrogen peroxide and ultraviolet light were found to be most effective if proper fit and seal were maintained.
More information: Emerging Infectious Diseases (2020). DOI: 10.3201/eid2609.202267
Journal information: Emerging Infectious Diseases
Provided by Marshall University Joan C. Edwards School of Medicine