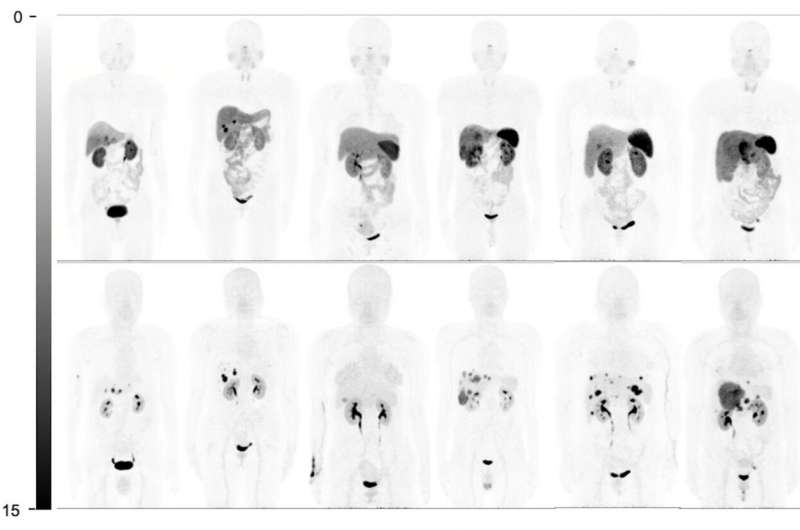
Comparison of whole-body maximum-intensity projections in 6 representative patients (patients 7, 8, 11, 14, 27, and 29 from left to right). Physiologic uptake is seen at pituitary gland, salivary glands, thyroids, adrenal glands, spleen (splenectomy in patients 7 and 8), and bowel on 68Ga-DOTATATE maximum-intensity projections (top). However, these normal organs show none or very mild uptake on 68Ga-DOTA-JR11 maximum-intensity projections (bottom). In addition, 68Ga-DOTA-JR11 depicts more liver lesions than 68Ga-DOTATATE, with lower liver background. Credit: Wenjia Zhu and Li Huo, et al., Peking Union Medical College Hospital, Beijing, China.
For neuroendocrine cancer patients with liver metastases, a new radiopharmaceutical, 68Ga-DOTA-JR11, has shown excellent imaging performance in tumor detection, staging and restaging, providing important information to guide treatment. In a head-to-head comparison of two somatostatin receptor (SSTR) imaging agents, 68Ga-DOTA-JR11 PET/CT performed better than 68Ga-DOTATATE PET/CT in detecting liver metastases, with a better tumor-to-background ratio, according to research published in the June issue of The Journal of Nuclear Medicine.
SSTRs—the key target for imaging and peptide receptor radionuclide therapy in patients with neuroendocrine tumors—typically are imaged using 68Ga-labeled peptides, which are agonists that bind to SSTRs to elicit a response. However, newly developed peptide antagonists, which recognize and then block SSTRs, have shown more favorable pharmacokinetics, better image contrast, higher tumor uptake, and better residence time in recent studies.
"With antagonists, we now have an alternative to agonists," stated Wenjia Zhu, MD, nuclear medicine physician, at Peking Union Medical College Hospital in Bejing, China. "However, there is still not much evidence about the performance of PET/CT imaging with SSTR antagonists. Hence, we designed this prospective study to compare 68Ga-DOTATATE and 68Ga-DOTA-JR11 PET/CT in patients with metastatic, well-differentiated neuroendocrine tumors."
The study included 31 patients and took place on two consecutive days. Each patient received an intravenous injection of 68Ga-DOTATATE on the first day and 68Ga-DOTA-JR11 on the second day. Whole-body time-of-flight PET/CT scans were performed 40-60 minutes after each injection on the same scanner. Upon completion, physiologic normal-organ uptake, lesion numbers, and lesion uptake were compared between 68Ga-DOTATATE and 68Ga-DOTA-JR11 PET/CT images.
The physiologic normal-organ uptake of the spleen, renal cortex, adrenal glands, pituitary glands, stomach wall, normal liver parenchyma, small intestine, pancreas, and bone marrow was significantly lower on 68Ga-DOTA-JR11 PET/CT than on 68Ga-DOTATATE PET/CT. 68Ga-DOTA-JR11 was found to detect significantly more liver lesions than 68Ga-DOTATATE; however 68Ga-DOTATATE detected more bone lesions than 68Ga-DOTA-JR11. While the radiopharmaceuticals showed similar lesion uptake for primary tumors and lymph node metastases on both patient-based and lesion-based comparisons, the target-to-background ratio of liver lesions was significantly higher on 68Ga-DOTA-JR11.
"What we've learned from this study is that peptides matter," noted Zhu. "For patients with different metastatic patterns, different peptides (DOTA-JR11 versus DOTATATE) should be used. In liver-dominant disease, 68Ga-DOTA-JR11 may be a better choice in tumor staging and restaging compared to 68Ga-DOTATATE. It may also change the treatment strategy, especially when partial resection or local therapy for liver metastasis is considered. In bone-dominant disease, we should probably stick to agonists, as 68Ga-DOTA-JR11 may underestimate tumor burden. We expect more extensive theranostic application of antagonists in the near future."
More information: Wenjia Zhu et al, Head-to-Head Comparison of 68Ga-DOTA-JR11 and 68Ga-DOTATATE PET/CT in Patients with Metastatic, Well-Differentiated Neuroendocrine Tumors: A Prospective Study, Journal of Nuclear Medicine (2019). DOI: 10.2967/jnumed.119.235093
Journal information: Journal of Nuclear Medicine
Provided by Society of Nuclear Medicine and Molecular Imaging