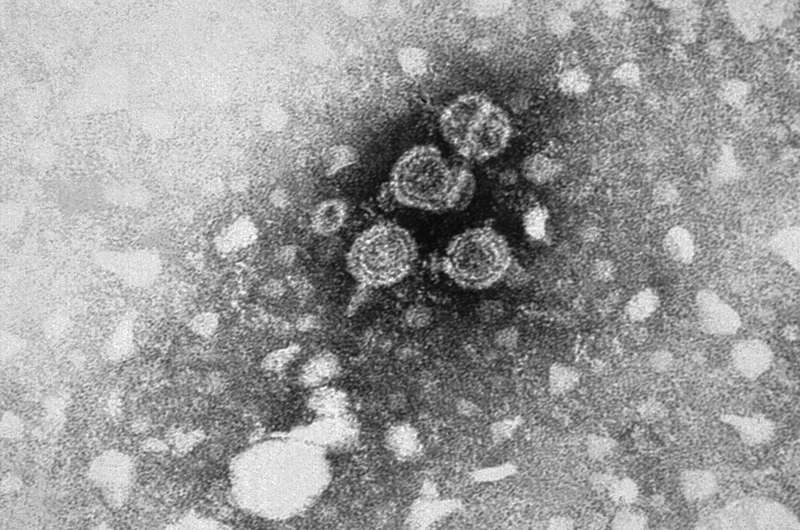
A microscopic image of the Hepatitis B virus, taken by the Centers for Disease Control and Prevention
Cost-effective ways to improve the delivery and management of hepatitis B (HBV) vaccine, identified in new Burnet Institute research, have attracted interest from global policy makers including the World Health Organization (WHO) and Gavi, the international vaccine alliance.
The Burnet study, published in The Lancet Global Health, recommends a review of controlled-temperature chain (CTC) refrigeration for HBV vaccine storage, and the adoption of easy-to-use compact pre-filled auto-disable (CPAD) devices in low- and middle-income countries (LMICs) to enable WHO to meet its global target of 90 percent birth dose HBV vaccination coverage by 2030.
HBV causes more than 800,000 deaths each year among the 257 million people globally who are chronically infected. Mother-to-child transmission is a major driver of HBV, with perinatal infection carrying the highest risk of cirrhosis, liver cancer and mortality.
Currently, only 44 percent of newborns in LMICs receive a timely dose of HBV vaccine, which is available in only 87 of 157 LMICs.
Modeling led by Burnet Ph.D. candidate Chris Seaman provides an economic argument for changes to CTC and CPAD interventions that would require higher up-front costs but prove extremely cost-effective in the long term.
"Pilot studies over decades suggest the hepatitis B vaccine may not require the stringent protocols around refrigeration that currently apply and may be robust enough to be stored at ambient temperatures for several weeks with no loss of efficacy," Mr Seaman said. "And the use of CPADs, which are safe and can be used by lay health workers, would obviate the need for trained health care workers to administer the vaccine using a needle and syringe."
He adds, "Our work addresses these logistical barriers and demonstrates that new interventions can provide significant cost-savings in low- and middle-income countries where they're really needed. This is about making optimal use of all of the vaccine's properties and potential and promoting early intervention to save the ongoing costs of managing a chronic disease."
Joint senior author, Burnet Institute Econometrician Dr. Nick Scott, said the existing protocols are a hindrance to birth dose coverage, which would likely reach a maximum of 65 percent in LMICs, well short of the WHO target of 90 percent, without a change in policy.
"WHO and Gavi understand that the barrier to getting this done is a change in policy," Dr. Scott said. "WHO has a Working Group looking into removing vaccines from the cold chain for these purposes, but what they haven't had until now is modeling evidence showing that global hepatitis B birth dose vaccination targets are unreachable without this change."
He explains, "The evidence that this paper provides, showing that the status quo is not good enough, is what they can use to get leverage to introduce policy changes. Now they have the numbers to show how important it is, as well as highly cost-effective and practical solutions."
More information: Christopher P Seaman et al. Use of controlled temperature chain and compact prefilled auto-disable devices to reach 2030 hepatitis B birth dose vaccination targets in LMICs: a modeling and cost-optimisation study, The Lancet Global Health (2020). DOI: 10.1016/S2214-109X(20)30231-X
Journal information: The Lancet Global Health
Provided by Burnet Institute