Credit: CC0 Public Domain
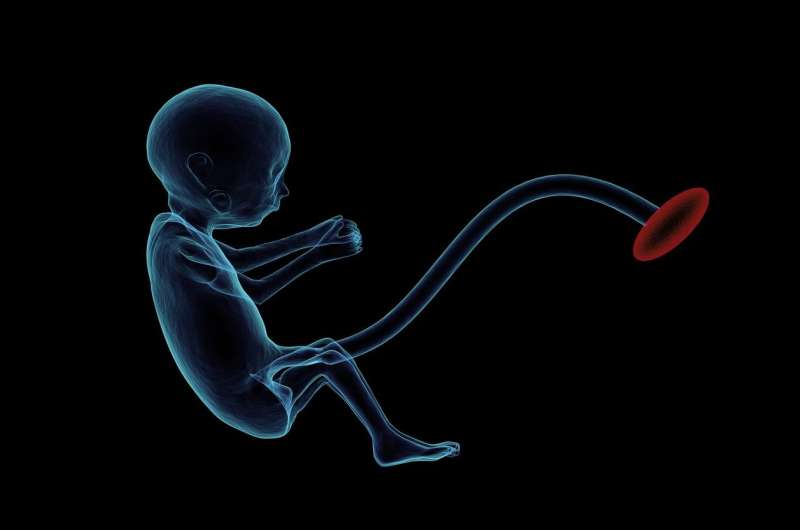
A baby girl in Texas—born prematurely to a mother with COVID-19—is the strongest evidence to date that intrauterine (in the womb) transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) can occur, reports The Pediatric Infectious Disease Journal, the official journal of The European Society for Paediatric Infectious Diseases.
The findings "suggest in utero transmission" of COVID-19 from an infected mother to her infant, according to the case report by Julide Sisman, MD, and colleagues of The University of Texas Southwestern Medical Center, Dallas.
"Numerous infants have now been delivered to pregnant women diagnosed with SARS-CoV-2, with the majority of these infants without respiratory illness or positive molecular evidence for SARS-CoV-2," comments Amanda S. Evans, MD, one of the lead authors of the new study. "Our study is the first to document intrauterine transmission of the infection during pregnancy, based on immunohistochemical and ultrastructural evidence of SARS-CoV-2 infection in the fetal cells of the placenta."
First Documented Intrauterine Transmission of COVID-19
The authors report on an infant delivered to a mother diagnosed with COVID-19, who also had type 2 diabetes. The infant was born at 34 weeks' gestation after the mother had premature rupture of the membranes. The baby was born "large for gestational age" (LGA) - an important complication in infants of diabetic mothers. She was treated in the neonatal ICU due to prematurity and possible SARS-CoV-2 exposure.
The infant appeared initially healthy, with normal breathing and other vital signs. On the second day of life, she developed fever and relatively mild breathing problems. "It is unlikely that the respiratory distress observed in this infant was due to prematurity since it did not start until the second day of life," the researchers write.
The baby tested positive for SARS-CoV-2 infection at 24 and 48 hours after birth. She was treated with supplemental oxygen for several days but did not need mechanical ventilation. COVID-19 tests remained positive for up to 14 days. At 21 days, the mother and infant were sent home in good condition.
The researchers examined the placenta, which showed signs of tissue inflammation. In addition, specialized tests documented the presence of coronavirus particles as well as a protein (SARS-CoV-2 nucleocapsid protein) specific for the COVID-19 virus in fetal cells of the placenta. Together, these findings confirmed that the infection was transmitted in the womb, rather than during or after birth.
Although data on COVID-19 remain very limited, "Intrauterine transmission of SARS-CoV-2 appears to be a rare event," Dr. Sisman and colleagues conclude. They highlight several urgent priorities for further research, including the mechanisms and risk factors of in utero SARS-CoV-2 transmission and the outcomes of congenital COVID-19 in infants.
"We wanted to be very careful of our interpretation of this data, but now is an even more important time for pregnant women to protect themselves from COVID-19," comments Dr. Evans. She adds, "The CDC has thoughtful guidance on ways to reduce risk of infection." (See https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/pregnancy-breastfeeding.html)
Two additional case reports in PIDJ also describe "vertical" transmission of SARS-Co-V2 from mother to infant occurring under different circumstances. Together, the three cases highlight the important but difficult distinction between virus transmission occurring before or during/after delivery (intrauterine versus intrapartum), according to a commentary led by George K. Siberry, MD, of the US Agency for International Development and Associate Chief Editor of PIDJ. Dr. Siberry and coauthors write: "As these cases illustrate, evaluation for vertical—and especially intrauterine—SARS-CoV-2 infection can be challenging, and assessment is often limited by lack of optimal testing of appropriate specimens obtained at specific timepoints."
More information: Julide Sisman et al, INTRAUTERINE TRANSMISSION OF SARS-COV-2 INFECTION IN A PRETERM INFANT, Pediatric Infectious Disease Journal (2020). DOI: 10.1097/INF.0000000000002815
Journal information: Pediatric Infectious Disease Journal
Provided by Wolters Kluwer Health