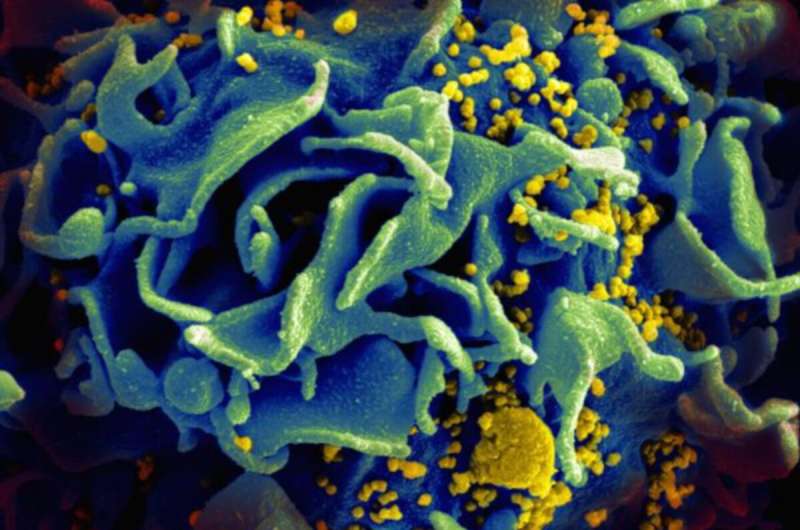
Microscopic image of an HIV-infected T cell. Credit: NIAID
A pre-exposure prophylaxis (PrEP) regimen containing an investigational long-acting form of the HIV drug cabotegravir injected once every 8 weeks was more effective than daily oral Truvada at preventing HIV acquisition among cisgender men who have sex with men and transgender women who have sex with men in a clinical trial sponsored by the National Institutes of Health. While both methods were highly effective for HIV prevention in the study population, the final data analysis indicated that cabotegravir had a superior protective effect. Findings from the Phase 2b/3 study, called HPTN 083, will be discussed in an online press conference and oral presentations during the 23rd International AIDS Conference (AIDS 2020: Virtual).
The only currently licensed PrEP medications—daily oral pills containing the HIV drugs tenofovir and emtricitabine—are highly effective at preventing HIV when taken as prescribed. However, taking a pill daily can be challenging. A long-acting form of PrEP could offer a less frequent, more discreet option that may be more desirable for some people. HPTN 083 and an ongoing companion study called HPTN 084, which is evaluating long-acting injectable cabotegravir for HIV prevention in cisgender women in sub-Saharan Africa, are sponsored by NIH's National Institute of Allergy and Infectious Diseases (NIAID).
In May 2020, a planned interim review of HPTN 083 data indicated a high level of efficacy for long-acting injectable cabotegravir among cisgender men and transgender women who have sex with men. The results reported today are based on a more extensive analysis of interim data from 4,566 study participants.
Overall, the rate of HIV acquisition in the participants was low. Among the 52 participants who acquired HIV, 13 were in the study group who received the cabotegravir-based PrEP regimen plus placebo daily oral tablets, and 39 were in the group who received daily oral Truvada plus placebo injections. This translated to an HIV incidence rate of 0.41% (95% confidence interval [CI] 0.22%-0.69%) in the cabotegravir group and 1.22% (95% CI 0.87%-1.67%) in the Truvada group—indicating 66% lower incidence in the cabotegravir group. Detailed analysis of these data indicated that the superior efficacy of cabotegravir was statistically significant.
Both products were safe and generally well-tolerated. Participants in the cabotegravir group were more likely to experience fever and pain or tenderness at the injection site compared to those in the Truvada group, who received placebo injections. Those in the Truvada group were more likely to report nausea. Most participants in the cabotegravir group received their injections as scheduled, with only 46 people (2.2%) discontinuing injections. Adherence to daily Truvada was also high, with 87% of a subset of 372 participants who provided blood samples having some detectable concentrations of the drug. Study investigators are continuing to follow the HPTN 083 study participants and to gather and analyze additional data on the long-term safety of injectable cabotegravir for HIV prevention.
More information: R. Landovitz et al. HPTN 083 interim results: pre-exposure prophylaxis containing long-acting injectable cabotegravir is safe and highly effective for cisgender men and transgender women who have sex with men. Oral presentation at the 23rd International AIDS Conference (AIDS 2020: Virtual), July 8, 5 p.m. EDT
B. Grinsztejn et al. HPTN 083 interim results: efficacy of pre-exposure prophylaxis containing long-acting injectable cabotegravir is maintained across regions and key populations. Oral presentation at the 23rd International AIDS Conference (AIDS 2020: Virtual), July 9, 4 a.m. EDT
Provided by National Institutes of Health