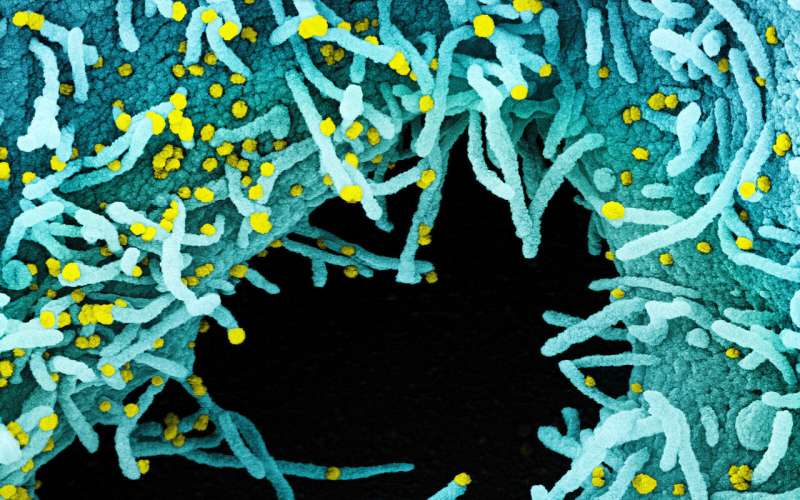
Colorized scanning electron micrograph of a cell infected with SARS-CoV-2 virus particles (yellow), isolated from a patient sample. Credit: National Institute of Allergy and Infectious Diseases, US National Institutes of Health
Like any other organism on the planet, the SARS-CoV-2 virus is prone to the natural genetic diversity that may arise from mutations. Since the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) hit the world, there have been fears that mutations could lead to more infectious or even more lethal strains of the coronavirus disease 2019 (COVID-19). Thankfully, the reverse may also be true.
With my colleagues at the Singapore Immunology Network (SIgN) and collaborators from institutes around Singapore, I investigated a genetic variant of SARS-CoV-2 that resulted in a less severe form of the disease, with a muted immune response, milder infections and better clinical outcomes. I will discuss our findings, which we published in The Lancet.
Genetic variation in SARS-CoV-2
There have been many variants identified in the SARS-CoV-2 genome. Because such genetic variation can translate to different features that affect the virus in different ways, there is interest in identifying the variants and their effects. For example, variants in immune targets or in regions of the virus that are targeted by diagnostic tests could have some serious effects on our fight against the virus. Genetic variations may also affect how transmissible and virulent the virus is, sparking fears of more dangerous strains.
We focused our study on a particular variant that was detected through the routine sequencing of the SARS-CoV-2 genome in a cluster of cases in Singapore that occurred between January and February of this year. This sequencing was done at Duke-NUS Medical School and also at the National Public Health Laboratory (NPHL), part of the National Centre for Infectious Diseases at Singapore's Ministry of Health.
This variation is a deletion of 382 nucleotides, which is why we refer to it as the ∆382 variant. The deletion is located in a region of the genome called the open reading frame 8 (ORF8) region, a known hotspot for mutations and genetic variation in coronaviruses. In this case, the deletion has resulted in the removal of the ORF8 transcription-regulatory sequence, meaning the ORF8 protein is not produced.
Back during the 2002-03 SARS epidemic, a deletion of 29 nucleotides in ORF8 resulted in a variant of the virus that was unable to replicate as efficiently as the wild-type virus. This observation led to some speculation that it could have resulted in a milder illness as well, although it was not examined at the time.
We decided it was worth looking into the ∆382 variant further. My colleagues at NPHL and Duke-NUS first screened 131 patients across seven Singaporean public hospitals with PCR-confirmed SARS-CoV-2 infections and found that the variant was present in about 30% of the patients. Of those 131 patients, 29 (22%) carried only the ∆382 variant virus, while 10 (8%) had a mix of both the wild-type and the ∆382 variant viruses. Similar variants with deletions of varying lengths in ORF8 have been observed in other countries as well, such as Bangladesh, Australia and Spain.
The deletion in action
Given what we know about the ORF8 region and the similar deletion in the SARS-CoV, we wanted to determine if the ∆382 variant affected the severity of subsequent SARS-CoV-2 infection. So the doctors on our team looked at the clinical features of the patients, using the patients' need for supplemental oxygen as a measure of infection severity to compare the patients infected with the variant against those infected with the wild-type SARS-CoV-2 virus.
Interestingly, patients with the ∆382 variant were less likely to need supplemental oxygen. Although all patient groups developed pneumonia at a similar rate, no patients in the ∆382-variant only group required supplemental oxygen. They were also less likely to develop hypoxia, the dangerous state of oxygen deprivation that arises in severe COVID-19 cases.
Not only that, but patients infected with the Δ382 variant also had lower concentrations of pro-inflammatory cytokines and chemokines that are strongly associated with severe COVID-19. Notably, they displayed lower concentrations of growth factors associated with lung injury and regeneration, suggesting that the infection was not severe enough to damage the lungs.
The patients with the Δ382 variant also had a better immune response: further immunological analysis revealed that they had more effective platelet regulation and T cell responses in the early phase of the infection, something usually severely impaired in SARS-CoV-2 infection. Instead, patients with the variant showed a more robust production of a cytokine called IFN-γ, which could be the reason for the rapid and effective immune responses observed.
These observations held true even after we re-classified the patient group for age and the presence of comorbid conditions. Because of this, we suspect that this variant somehow triggers a reduced pro-inflammatory response and a lower, less damaging cytokine storm that resulted in a milder form of the COVID-19 disease.
Our observations and findings support the suggestion that the ∆382 variant of SARS-CoV-2 is associated with a milder infection and better clinical outcomes. However, we do not yet know why this is so. Unlike the 29-nucleotide deletion in the SARS-CoV virus, tests have shown that the Δ382 variant does not affect how well the SARS-CoV-2 virus replicates, as evidenced by the similar viral loads observed in patients with and without the ∆382 variant.
It could be the ORF8 protein, although the exact function of this protein in SARS-CoV-2 remains unclear. However, there is evidence to suggest that it plays an important role. One study has suggested that it may help the virus evade immune detection, while another has indicated that ORF8 is frequently an early target for human antibodies during SARS-CoV-2 infection. Considering all this, we speculate that ∆382 variants might be less effective at establishing infection in a new host because of the loss of the immune evasion functions conferred by ORF8. Therefore, potential therapeutic strategies could consider inhibiting ORF8.
Hope for the future
So what does it all mean? It is interesting to speculate how a deeper understanding of these genetic variants could help future treatments or vaccines to exploit them. If deletions in ORF8 really translate to the milder infection as they do in the ∆382 variant, it could have implications for the development of vaccines, for instance. As it gives rise to a less severe form of the infection and an efficient immune response, this natural variant could serve as an attenuated live vaccine.
In the future, my team and I would like to work to decipher the molecular mechanisms of the variants that drive the different immune responses. For now, I want to credit my collaborators at the National Centre for Infectious Diseases, the Ministry of Health, Duke-NUS Medical School, and A*STAR's Infectious Diseases Horizontal Technology Centre (ID HTC) and Bioinformatics Institute (BII) for their work on this paper, from collecting the clinical samples to conducting the experiments and analyzing the data.
More information: Barnaby E Young et al. Effects of a major deletion in the SARS-CoV-2 genome on the severity of infection and the inflammatory response: an observational cohort study, The Lancet (2020). DOI: 10.1016/S0140-6736(20)31757-8
Journal information: The Lancet