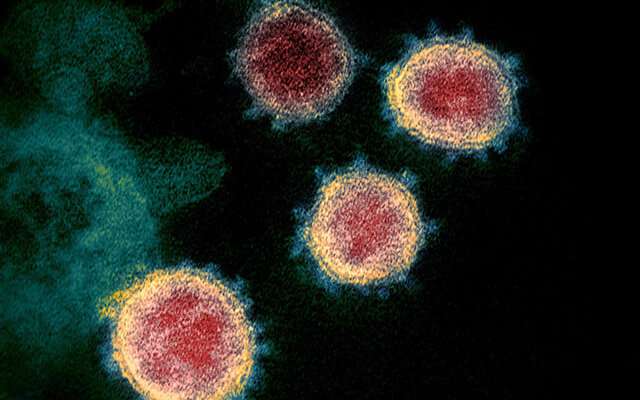
A colorized scanning electron micrograph of the SARS-CoV-2 virus. Credit: NIAID
One test of both the power and hunger of any individual or organization is the ability to master any and every new, sufficiently advanced technological opportunity that urgently presents itself to the world at large. For example, when smartphones first materialized, these kinds of folks wouldn't rest until they had created basic apps for themselves. And when the powerful new CRISPR technology became available, neither did any rest until they had experimented with the gene editing technology for themselves. In other words, for them, the gift and curse is that it is simply more painful not to know exactly how it is done than it is to be deprived of basic physical comforts.
Biological problems are fundamentally different from many man-made technologies in that the solutions are not just hard to access, they often don't yet even exist. They must be created from scratch rather than looked up and copied. A case in point is the current COVID-19 pandemic. Massive amounts of data associated with COVID-19 have accumulated over the past several months. Deriving actionable knowledge from this data has now become the premiere challenge of the day to all comers big and small.
A company called nference has recently developed a software platform with the stated goal of synthesizing all the world's biomedical knowledge. When the epidemic began, they rose to the challenge and rapidly pivoted to produce paper after groundbreaking paper uncovering key aspects of the disease. I recently spoke with co-founder & Chief Scientific Officer Venky Soundararajan and Director of Scientific Research AJ Venkatakrishnan about several of these new papers, including their most recent one, published Monday in eLife.
This paper addresses an increasingly important aspect of COVID-19 pathology: the so-called COVID-associated coagulopathies (CAC). Hypercoagulability, in particular, is a major concern in the acute respiratory distress (ARDs) seen in the severest cases of COVID-19. The question naturally arises as to whether the severe COVID-19 symptoms might involve, and therefore be treated similarly to, the well-known phenomenon of disseminated intravascular coagulopathy (DIC). In DIC, the delicate balance normally maintained between coagulation and fibrinolysis becomes severely dysregulated.
Typically, blood clots caused by DIC form throughout the body, primarily within the small blood vessels. Then, as the various clotting factors are consumed and depleted, bleeding begins to occur. The condition is therefore often called a consumption coagulopathy. No one single marker reliably captures a case of DIC. Instead, a constellation of laboratory values taken together over time, together with a consistent medical history, is often needed to evaluate the condition properly. The treatment regimen has similarly become more complex over time, precisely tailoring different amounts of an increasing palette of natural and artificially produced factors in each case.
The authors of the nference eLife paper studied 246 COVID-19 patients and 2,460 COVID-19-negative patients subjected some 700,000 lab tests cumulatively across 194 assays. They found that plasma fibrinogen was significantly elevated in COVID-19 patients at the time of diagnosis, but hyperfibrinogenemia generally resolved by seven days after diagnosis. Platelet counts were lower in the COVID-19 cohort at the time of clinical presentation but then increased over the next 10 days to levels above the COVID-19 negative patients. A partial higher thromboplastin time (aPTT) was also observed in the COVID-19 patients, but levels of D-dimer (a fibrin degradation fragment produced where blood clots dissolve) were comparable.
The authors then used a neural network to evaluate whether the observed coagulation-related laboratory trends were associated with clinical manifestations of thrombosis. The analysis confirmed that a DIC-like coagulopathy with hemorrhage and thrombosis can develop in COVID-19, but it is rare—only five of the 2,232 COVID patients were formally diagnosed. Therefore, although platelet counts, fibrinogen levels and clotting time in COVID patients can resemble DIC, we are dealing with a different kind of disease.
In another recent eLife paper, the authors used their platform to conduct a comprehensive expression profiling of ACE2 across host tissues and cell types, which they then correlated with COVID-19 pathogenicity and viral transmission. To do this, they scanned 100 million biomedical documents to generate conceptual associations from single-cell RNA sequencing, bulk RNA-seq and proteomics. They identified tongue keratinocytes and olfactory epithelia as novel ACE2-expressing cell populations and important potential sites of SARS-CoV-2 infection. The molecular fingerprint they established is a striking correlate to recent clinical reports of dysgeusia and anosmia (disrupted sense of taste and smell, respectively).
In a third paper for eLife, Venky, AJ, and others reported that SARS-CoV-2 has evolved a unique S1/S2 cleavage site not found in any previously sequenced coronavirus, which results in the striking mimicry of an identical FURIN-cleavable peptide found on a human epithelial sodium channel known as ENaC-α. The authors suggest that the evolution of COVID into a global pandemic may have been driven in part by the targeted mimicry of this ENaC-αchannel. In humans, the channel is critical for the homeostasis of airway surface liquid, and its misregulation is associated with respiratory conditions.
Together, these diverse papers constitute a substantial new contribution to our understanding of COVID-19, and form a solid base for future studies using the nference software platform.
More information: Colin Pawlowski et al. Inference from longitudinal laboratory tests characterizes temporal evolution of COVID-19-associated coagulopathy (CAC), eLife (2020). DOI: 10.7554/eLife.59209
AJ Venkatakrishnan et al. Knowledge synthesis of 100 million biomedical documents augments the deep expression profiling of coronavirus receptors, eLife (2020). DOI: 10.7554/eLife.58040
Praveen Anand et al. SARS-CoV-2 strategically mimics proteolytic activation of human ENaC, eLife (2020). DOI: 10.7554/eLife.58603
Journal information: eLife
© 2020 Science X Network