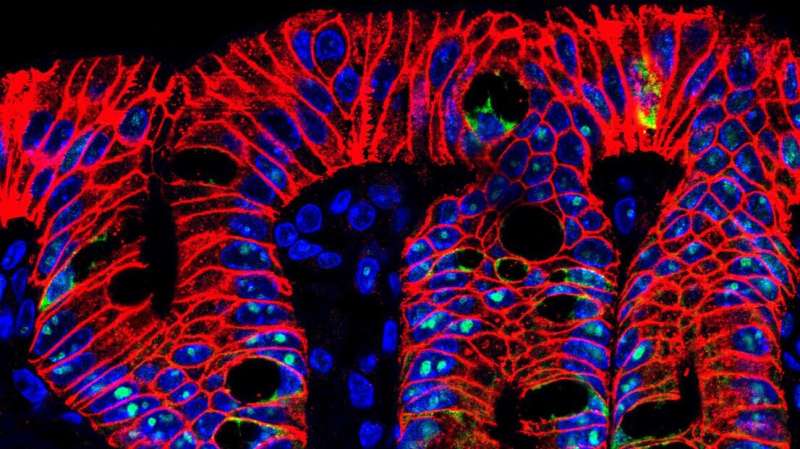
Mouse intestinal crypts. Credit: K. Schoonjans (EPFL)
Researchers at EPFL have made a surprising discovery about how bile acids act as signaling molecules to boost intestinal regeneration. The discovery sheds light on the role of bile acids as hormone-like molecules and opens new ways for regenerative therapies of the gut.
Intestinal stem cells replenish the cells lining the gut epithelium, which usually renews itself every week. These cells also generate all the specialized cells of the gut that carry out different functions e.g. antimicrobial protection, mucus secretion, and the release of nutrient-induced hormones. When injury occurs, the intestinal stem cells become activated and coordinate the repair of the damaged epithelium and the recovery of intestinal function.
A team of scientists led by Kristina Schoonjans at EPFL have discovered that exposing stem cells to physiological concentrations of bile acids can boost the growth of miniature "guts" called organoids. On the cutting-edge of bio-engineering, gut organoids are grown from isolated intestinal stem cells in the lab as tiny, three-dimensional tissues that simulate the anatomy and function of many cell types found in the actual gut.
The scientists found that exposing intestinal cells to bile acids not only helped them grow into organoid intestines, but also preserved their ability to differentiate into specialized cell types. Bile acids even increased the number of cells that secrete glucagon like peptide-1 (GLP-1), an important gut hormone with established antidiabetic actions.
In addition, they discovered that the bile acid-activated membrane receptor, called TGR5, is enriched in intestinal stem cells, and that it contributes to their activation when bile acid levels accumulate in the gut, e.g. after eating a meal.
Looking deeper into their findings, the researchers generated genetically modified mice to disrupt the function of TGR5 specifically in intestinal stem cells. The result was that bile acids not only increased the number of intestinal stem cells in the mice's gut, but also protected mice from acute colitis by promoting intestinal regeneration through a mechanism that involves TGR5.
"The results of our work imply that every time we eat—a process that triggers the secretion of bile acids into the gut—we are stimulating the regeneration and the proper functions of the intestine, through the action of bile acids on intestinal stem cells," says Schoonjans.
"However, our study also includes a warning: dietary habits known to chronically increase the levels of bile acids into the gut, such as the consumption of high-fat food, might exacerbate intestinal stem cell proliferation and transform the homeostatic intestinal regeneration into cancer development."
The researchers hope that, in the future, the administration of synthetic molecules that can activate TGR5 specifically in the gut, might become a pharmacological strategy to acutely stimulate the regeneration of damaged intestinal epithelium in patients with inflammatory bowel disease.
More information: Giovanni Sorrentino et al. Bile Acids Signal via TGR5 to Activate Intestinal Stem Cells and Epithelial Regeneration, Gastroenterology (2020). DOI: 10.1053/j.gastro.2020.05.067
Journal information: Gastroenterology
Provided by Ecole Polytechnique Federale de Lausanne