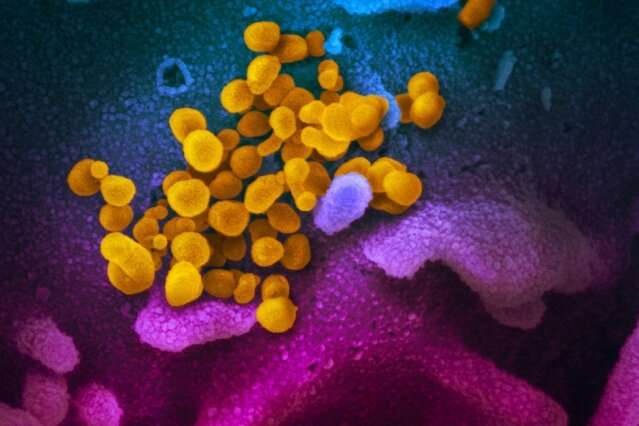
This scanning electron microscope image shows SARS-CoV-2 (yellow)—also known as 2019-nCoV, the virus that causes COVID-19—isolated from a patient, emerging from the surface of cells (blue/pink) cultured in the lab. Credit: NIAID-RML
A study of interim data from two hospitals in an early US COVID-19 hotspot, to be presented at the ESCMID Conference on Coronavirus Disease (ECCVID, held online 23-25 September), shows that race and ethnicity were not significantly associated with higher in-hospital COVID-19 mortality, and that rates of moderate, severe, and critical forms of COVID-19 were similar between racial and ethnic groups.
The study, by Dr. Daniel Chastain (University Of Georgia College Of Pharmacy, Albany, GA, U.S.) and colleagues included data from adult patients hospitalised between March 10 and and May 22 with COVID-19, defined by laboratory-detected severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, in Southwest Georgia.
The authors compared severity of illness categories on presentation to the hospital between patients from different racial and ethnic groups based on criteria from the US National Institutes of Health (NIH) COVID-19 treatment guidelines. They also studied outcomes including comorbidities, laboratory values, vital signs, and in-hospital mortality.
A total of 164 randomly selected non-consecutive patients were included with a median age of 61.5 years. These consisted of 119 African American patients, 36 Caucasian patients, and 9 Latinx patients. Thus the majority were African American (73%) and 51% were female. Rates of moderate, severe, and critical COVID-19 did not significantly differ between African American (9%, 56%, and 35%), Caucasian (0%, 69%, and 31%), and Latinx patients (0%, 56%, and 44%). In-hospital mortality was not statistically significantly different between groups but was highest among Caucasians (31%) followed by Latinx (22%) and African Americans (16%).
Caucasian patients had significantly higher Charlson comorbidity index scores (meaning more underlying conditions) (4.5) compared to African American (4) and Latinx (2) patients, while median BMI was significantly higher in African Americans (33.7 kg/m2) than in Caucasians (26.9) or Latinx patients (25.9).
Duration of time from symptom onset to admission was similar between groups, whereas median temperature on admission was significantly higher in African Americans (38.3C) than in Caucasians (37.9) or Latinx patients (37.8)
The authors conclude: "Despite the majority of our cohort being African American, the rates of moderate, severe, and critical forms of COVID-19 were similar between racial and ethnic groups in a major transmission hotspot during the early spread of the pandemic in the Southeastern US. Race and ethnicity were not significantly associated with higher in-hospital mortality...our results were similar to findings from other recent studies from the states of Massachusetts and Louisiana. However, since this is an interim analysis, there is a possibility that these results were due to chance. We are in the process of conducting additional follow-up studies with a larger sample size."
More information: academic.oup.com/cid/advance-a … cid/ciaa1245/5896009
Provided by European Society of Clinical Microbiology and Infectious Diseases