Gene could slow down tumor repair in breast cancer brain metastasis
Treating tumors presents a tricky conundrum: a higher dose of radiation is more effective for treatment, but the higher the dose, the more danger it poses to healthy cells.
Researchers at Yale have made significant inroads into solving this problem in a paper titled, "LRRC31 inhibits DNA repair and sensitizes breast cancer brain metastasis to radiation therapy," published in Nature Cell Biology on October 1, 2020. Principal investigator Dr. Jiangbing Zhou, Ph.D., associate professor of neurosurgery and of biomedical engineering at Yale School of Medicine, and his team, describe a unique finding in the study: the targeted delivery of specially engineered nanoparticles loaded with a gene that could make breast cancer brain metastases (brain tumors that originate from breast cancer) more sensitive to radiation therapy. They report that the procedure significantly improved the survival rate of tumor-bearing mice after they were treated with radiation.
Breast cancer brain metastasis (BCBM) happens to between 10 and 15 percent of people suffering from stage 4 breast cancer, with the five-year survival rate being 22 percent. Radiation therapy is the standard treatment of BCBM but delivering safe amounts of radiation strong enough to kill the cancer cells is a delicate balance. This is because an inherent mechanism in most cells causes them to start the repair process once hit with radiation. Thus, a radiation dose high enough to fully destroy a cancer cell and keep it from repairing itself is needed, but that would mean also threatening healthy cells.
One way to reduce the amount of radiation required would be to find a way to slow down or stop the tumor cells' repair mechanism without affecting healthy cells. To do so, Dr. Zhou's team used the gene-editing technology CRISPR to zero in on a gene called the leucine-rich repeat-containing protein 31 (LRRC31). This protein turns out to be the most efficient radio-sensitizing gene for these types of cancer cells.
Once the LRRC31 gene was identified, researchers were faced with the challenge of delivering it to the tumor sites in the brain. This is because the blood–brain barrier (BBB) prevents potentially dangerous substances, including drugs used in chemotherapy, from crossing over from the bloodstream to the brain. Although metastatic tumors partially disrupt the BBB, it remains intact enough to thwart most therapeutics.
"Drug delivery to the brain is very difficult," says Dr. Zhou. "We used nanoparticles, which were engineered to cross the blood–brain barrier […] to target tumors in the brain." These LRRC31-loaded nanoparticles were developed by his lab and took advantage of the breaches in the BBB due to metastasis to access the tumor sites.
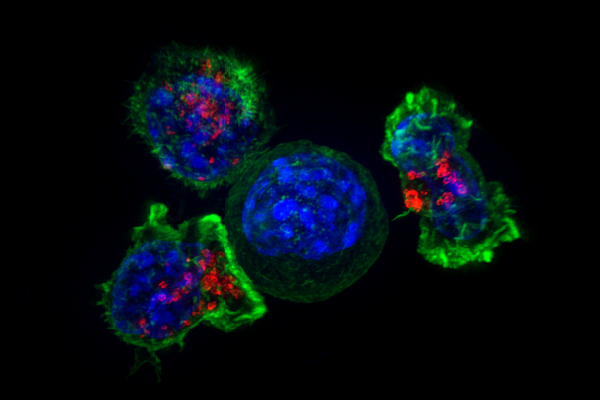
For their study, cells from human BCBM were transplanted into mice, who were then treated with the nanoparticles. The eventual goal, however, is to develop treatments that can be successful in humans. However, "translation to clinical treatment [for humans] always takes a long time," says Dr. Zhou. "How to enhance radiotherapy is the obvious one [and] we are working on that, but in terms of DNA repair, [that] plays a role in many other therapeutic regimens, like immunotherapy [or] genome-editing."
More information: Yanke Chen et al. LRRC31 inhibits DNA repair and sensitizes breast cancer brain metastasis to radiation therapy, Nature Cell Biology (2020). DOI: 10.1038/s41556-020-00586-6





















