Credit: Unsplash/CC0 Public Domain
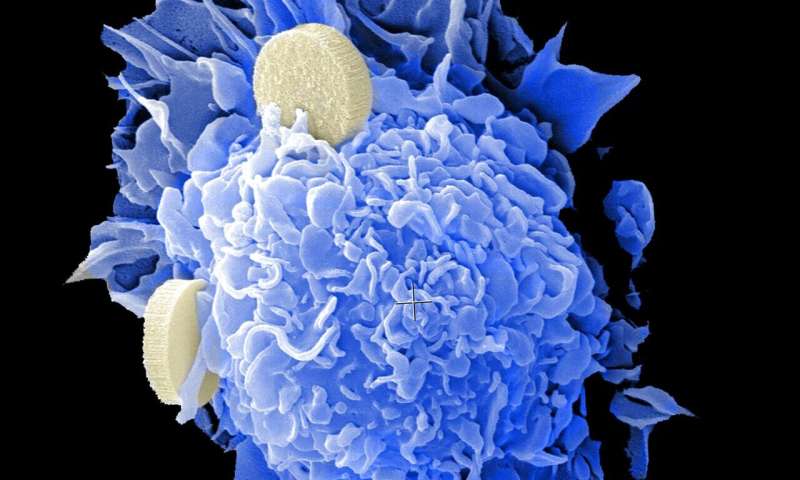
Cancer metastasis, which is the dissemination of tumor cells into distant organs, is the leading cause of mortality in cancer patients. To undergo metastasis, cells must leave the primary tumor, circulate into the blood, colonize distant organs, and form distant metastasis. It has been proposed that epithelial to mesenchymal transition (EMT), a process in which epithelial cells detach from their neighboring cells, and acquire mesenchymal migrating properties, is important to initiate the metastatic cascade allowing the cancer cells to leave the primary tumor. However, the role of genetic mutations in promoting EMT is unknown.
FAT1 is among the most frequently mutated driver genes in a broad range of human cancers. The loss of function mutations in this gene suggest that FAT1 acts as tumor suppressor, preventing cancer development. However, and despite the high frequency of FAT1 mutations, its role in cancer is poorly understood.
In a study published in Nature, researchers led by Prof. Cedric Blanpain, MD/Ph.D., WELBIO investigator, Director of the Laboratory of Stem Cells and Cancer and Professor at the Université libre de Bruxelles, Belgium, demonstrated, for the first time, that loss of FAT1, promote EMT, invasive features and metastasis in skin squamous cell carcinoma -the second most frequent cancer in humans-, lung cancer -the deadliest cancer—and head and neck tumors.
Ievgenia Pastushenko and colleagues used state of the art genetic models of skin and lung cancers, as well as human skin, lung and head and neck tumors to assessthe role of FAT1 in cancer.
The authors discovered that loss of function of FAT1, promotes hybrid EMT phenotype, characterized by the co-expression of epithelial and mesenchymal genes in tumor cells. The authors demonstrated that this hybrid EMTstate occurring following FAT1 loss of function, promotes metastasis and was associated with poor clinical outcome in patients with lung cancers. "It was particularlyexciting to identify that mutations in a single gene, FAT1, promote hybrid EMT state, leading to metastasis and associated with poor prognosis in cancer patients" comments Ievgenia Pastushenko, the first author of this study.
Using different molecular approaches, the authors decipher the mechanisms by which FAT1 mutations promote hybrid EMT state. "The identification of the mechanismsthat promote this highly metastatic tumor state, allowed us to identify drug resistance and vulnerabilities in FAT1 mutated cancers. We found that Fat1 mutated cancers arehighly resistant to several drugs including EGFR inhibitor that are frequently used to treat patients with lung cancers. Most interestingly, we identify that FAT1 mutated cancers are particularly sensitive to other drugs including Src inhibitor that are currently used to treat patients with blood cancer. These findings will have very important andimmediate implications for personalized therapy in patients FAT1 mutated cancers," comments Pr Cedric Blanpain, the senior author of this study.
More information: Ievgenia Pastushenko et al. Fat1 deletion promotes hybrid EMT state, tumour stemness and metastasis, Nature (2020). DOI: 10.1038/s41586-020-03046-1
Journal information: Nature
Provided by Université libre de Bruxelles