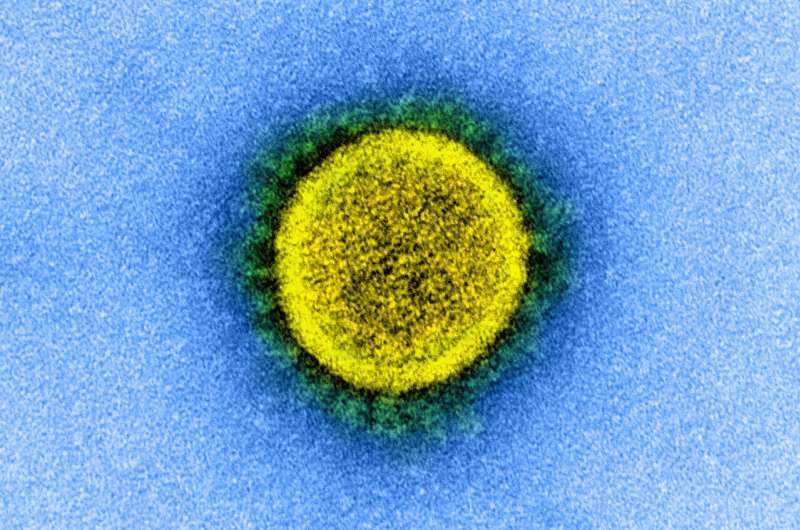
SARS-CoV-2 (shown here in an electron microscopy image). Credit: National Institute of Allergy and Infectious Diseases, NIH
Since its appearance in early 2020, COVID-19 has been unpredictable for both physicians and affected individuals given the variety and duration of its symptoms. Notably, it appears to have the potential to cause an unusually long-lasting illness, and the term "long COVID" describes the disease in people who continue to report symptoms several weeks following the infection. To better understand this phenomenon, a team of physicians and epidemiologists from the University of Geneva (UNIGE) the University Hospitals of Geneva (HUG) and the General Health Directorate of the State of Geneva followed nearly 700 people who tested positive for SARS-COV2 but did not require hospitalization. Six weeks after diagnosis, 33% of them still reported suffering from fatigue, loss of smell or taste, shortness of breath or cough. These results, which can be seen in the Annals of Internal Medicine, call for better communication, particularly with patients and with the physicians who follow them, and for ongoing messages to the general public, reminding them that SARS-CoV-2 infection is not trivial.
Even if in just a few months medical and scientific knowledge about SARS-COV2 has considerably improved, several aspects of this disease remain unknown. In particular, many people are wondering about the evolution and long-term consequences of this novel virus. "As soon as the pandemic arrived in our country, we were confronted with these questions," reports Professor Idris Guessous, physician epidemiologist at the Department of Community Health and Medicine of the UNIGE Faculty of Medicine and Chief Physician of the Division of Primary Care at HUG, who directed this work. "In March, the COVICARE program was set up to offer remote monitoring to patients who can be followed on an outpatient basis, when this follow-up could not be carried out by the primary care physician. This has enabled us to better understand the evolution of the disease in people who generally suffer neither from specific risk factors nor from a serious form of the disease."
Some Very Tired Patients
A total of 669 people were followed (mean age 43 years, 60% female, 25% of healthcare professionals and 69% without underlying risk factors that could be related to complications from COVID-19). At 6 weeks from diagnosis, nearly a third of participants still had one or more symptoms related to COVID-19, mainly fatigue (14%), shortness of breath (9%) and loss of taste or smell (12%). In addition, 6% reported a persistent cough and 3% reported headaches. Dr. Mayssam Nehme, Senior Resident in Professor Guessous's team and first author of this work, also explains how these patients felt: "In addition to the physical distress of their symptoms, many were very worried: how much longer would it last? Were some after-effects irrecoverable? Even without a clear medical answer, in the current state of knowledge, it is important to accompany concerned patients and to listen to them," she adds. With this in mind, the HUG has set up a specific consultation for long COVID patients in order to improve their care and guide them through the health system.
Better Understanding for Better Information
The persistence of symptoms must be recognized in order to legitimize the concerns of patients faced with a new and unknown disease, and to optimize their management. "This requires an information campaign towards the general public and healthcare workers, but also, more broadly, among employers, insurance companies and society in general. Everyone should realize that previously healthy people can also be affected by COVID-19, weeks or even months following the infection. Prevention is therefore of the utmost importance," add the authors, who are continuing their studies to understand the long-term evolution of these patients. Indeed, a follow-up of the same cohort 3 months, 7 months and 12 months following the infection is in progress.
More information: Mayssam Nehme et al, COVID-19 Symptoms: Longitudinal Evolution and Persistence in Outpatient Settings, Annals of Internal Medicine (2020). DOI: 10.7326/M20-5926
Journal information: Annals of Internal Medicine
Provided by University of Geneva